Last Updated on November 22, 2023
Spina bifida is a neural tube defect that leads to a congenital defect in the posterior bony wall of the spinal canal [vertebral arch] involving the laminae and spinal cord malformation. The condition has a spectrum of presentation that ranges from incidental finding on x-ray to stillbirth.
Spina bifida is most commonly seen in the lumbosacral region. Sometimes the contents of the canal may protrude through the defect.
The average reported incidence of spina bifida is 1 case per 1000 births. The rate may differ according to geographic variations occur.
The term bifida is derived from the Latin bifidus which means “in 2 parts.”
Development of the spinal cord
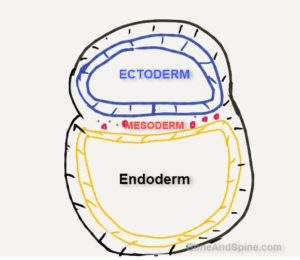
During the 2nd week of intrauterine life, the early embryo has three primitive layers separated as ectoderm, mesoderm and endoderm. Following diagram which represents a cut section will help to understand.
Ectoderm gives rise to the nervous system and skin.
Mesoderm mainly forms the skeletal muscles, smooth muscle, blood vessels, bone, cartilage, joints and other connective tissue.
The endoderm gives rise to the lining of the viscera and airways.
Thus spinal cord will originate from the ectoderm and vertebrae of the spine are formed from the mesoderm.
With this basic understanding, let us now focus on the development of the spinal cord.
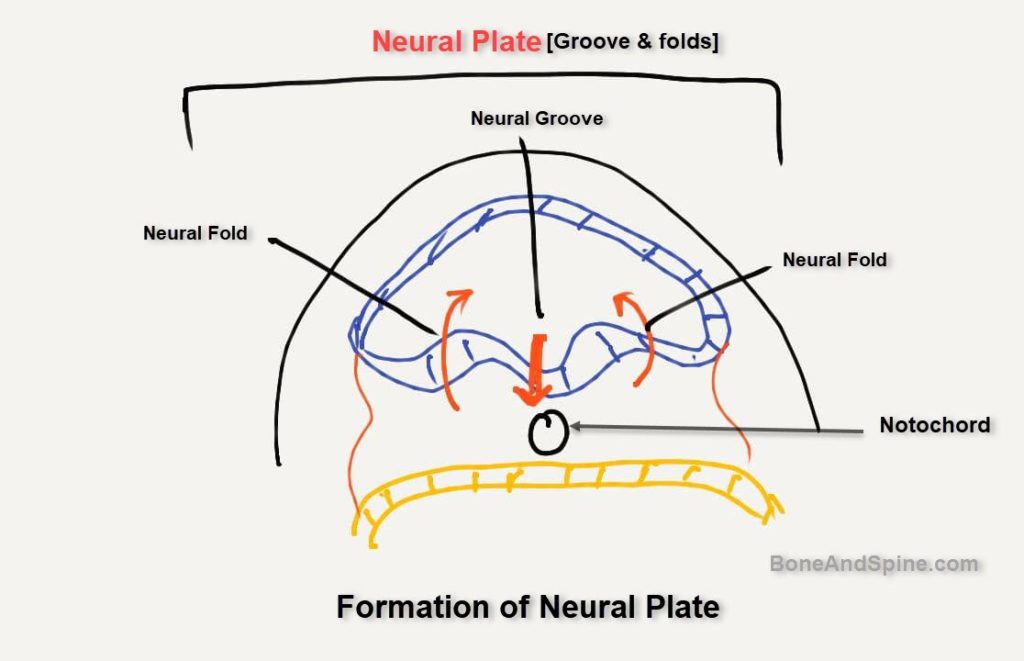
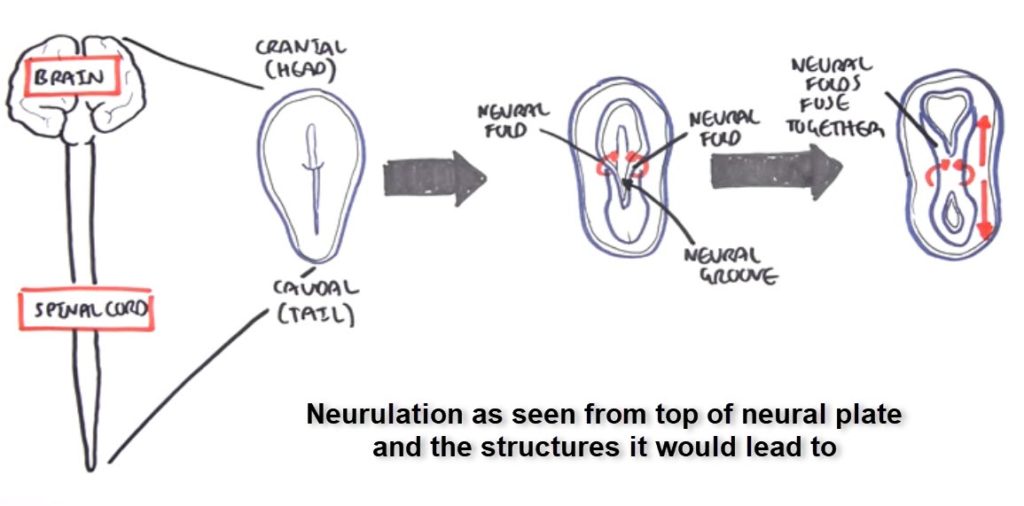
Neurulation is the name given to stage of the embryo when the formation of neural tube that would eventually form the the brain and spinal cord.
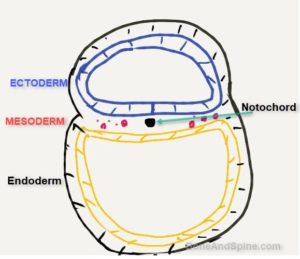
The notochord is flexible rod-like structure derived from the mesoderm. It serves as the basis of the axial skeleton. It also acts as an inducer of neurulation. It induces the overlying ectoderm to differentiate the part of the ectoderm[neuroectoderm] to differentiate into neural plate. It is a transient structure that finally becomes part of the nucleus pulposus of the adult disc.
A dorsal groove appears on the surface of the embryo, which is known as the neural groove. The raised cells on either side are called neural folds.
The folds rise to meet each other causing the margins of the neural groove unite into a tube known as the neural tube and the lumen, within it, is called the neural canal.
The neural tube becomes separated from the surface by an ingrowth of the mesoderm.
Also the ectodermal folds surround the endoderm and mesoderm to form an image like this. 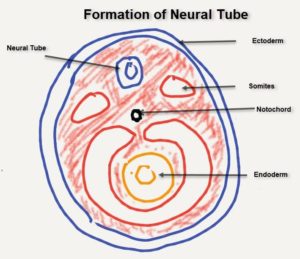
The mesoderm surrounds the endoderm and also gives a pair of somites along the neural tube. Somites will give rise to the vertebra and other musculoskeletal organs.
The process of neurulation begins in the middle and moves cranially [towards head] and caudally [towards tail literally or away from head]
The following diagram is the other view to understanding this process. This shows the process as viewed from the top of the neural tube.
In front of the neural tube, there is a solid rod of cells, known as the notochord. Around the notochord, the vertebral bodies develop.
Actually, notochord is the transient structure and responsible for induces neurulation. Later it becomes part of nucleus pulposus of the vertebral disk.
From each of the bodies, there extend two projections that grow around the neural tube to form the vertebral arch or neural arch.
Failure of fusion of these arches gives rise to spina bifida.
This video explains the formation of the spinal cord quite well.
Causes of Spina Bifida
Neural tube defects result from failed closure and abnormal differentiation of the embryonic neural tube. These occur between the 17th and 30th day of gestation.
Anencephaly and myelomeningocele are the most common neural tube defects.
Myelomeningocele occurs due to a failed closure of the caudal end of the neural tube resulting in a sac that contains dysplastic spinal cord, nerve roots, meninges, vertebral bodies, and skin.
Most infants born with spina bifida are born to mothers with no previously affected children
Spina bifida has multifactorial causation. Chromosomal abnormality is reported in 10% cases. Other factors are maternal risk factors. These are
main factors that are thought to be responsible are
- Folic acid deficiency [50% of cases are attributed]
- Pregestational diabetes – increases the risk of CNS malformation
- Maternal obesity
- Hyperthermia
- Maternal diarrhea
- Intrauterine exposure to antiepileptic drugs and drugs used to induce ovulation
- Maternal exposures to
- Fumonisins [toxins produced by fungi]
- Electromagnetic fields
- Hazardous waste sites
- Disinfection by-products found in drinking water
Associated Conditions
- Spine deformities- scoliosis, kyphosis, hemivertebra
- Lower limb deformities
- Hip dislocations and contractures
- Knee deformities- tibial torsion and contractures
- foot deformities
- Hydrocephalus
- Chiari II malformation- Lower brainstem and/or upper cervical spinal cord compression
- Short Stature
- Cranial nerve dysfunction – Ocular muscle palsies, dysphagia and dysphonia.
- Tethered spinal cord – pain, sensory changes, spasticity, and progressive scoliosis.
- Syringomyelia [dilatation of cord]
- Renal Problems
- Neurogenic bowel and bladder
- Bladder incontinence
- Hydronephrosis due to a contracted bladder
- Infections and renal failure
- Vesicoureteral reflux
- Congenital Abnormalities
- Facial clefts
- Heart malformations
- Pathologic fractures
Types of Spina bifida and Their Findings
Spina Bifida Occulta
Spina bifida occulta is characterized by
-
- Failure of the neural arches to unite
- No protrusion of the cord or membranes
- Small gap may be seen in the vertebral arch, the gap is filled with fibrous tissue.
- Usually affects vertebra is affected and the gap is filled with fibrous tissue.
- Usually without symptoms
The skin may show dimple, skin pigmentation, or a hairy patch. A spinal cord lipoma or a fibrous cord may be present underneath these subtle signs.
Problems with micturition or a foot deformity may be seen in some cases of occulta.
In later ages, the patient may present with tethered cord.
Many cases of spinal bifida occulta are symptomless. Either they remain undiagnosed or diagnosed by accident when an x-ray taken for some other reasons.
Spina bifida occulta is present since birth. A complete neurological examination must be performed for reocrd purpose and then at follow up at adolescence. These patients may develop backache, nocturnal enuresis, local anesthesia, local weakness or even foot drop.
At one stage the spinal cord reaches the distal end of the vertebral column. Gradually the cord lags behind in growth in comparison to the vertebral column in intrauterine life so that at birth the distal end of the cord lies at the third lumbar vertebra.
Later on, due to more development of the vertebral column, the distal end of the cord lies at the lower end of the first lumbar vertebra in adults. With the growth of the body, the membrana reunions pull on the theca and nerve roots. This causes some neurological deficiencies e.g. foot drop, nocturnal enuresis or a backache. Such symptoms appear late in childhood or in adult life.
X-ray is often confirmatory as it will show the bony defect.
A fibrous band, the membrana reunions connects the skin to the spinal theca.
Most of the patients do not require treatment. For cosmetic reasons, the tuft of hair or lipoma may be removed.
In tethered cord syndrome, the membrana reunions is excised. Extradural or intradural lipomas if present and causing compression of neural tissue should be excised.
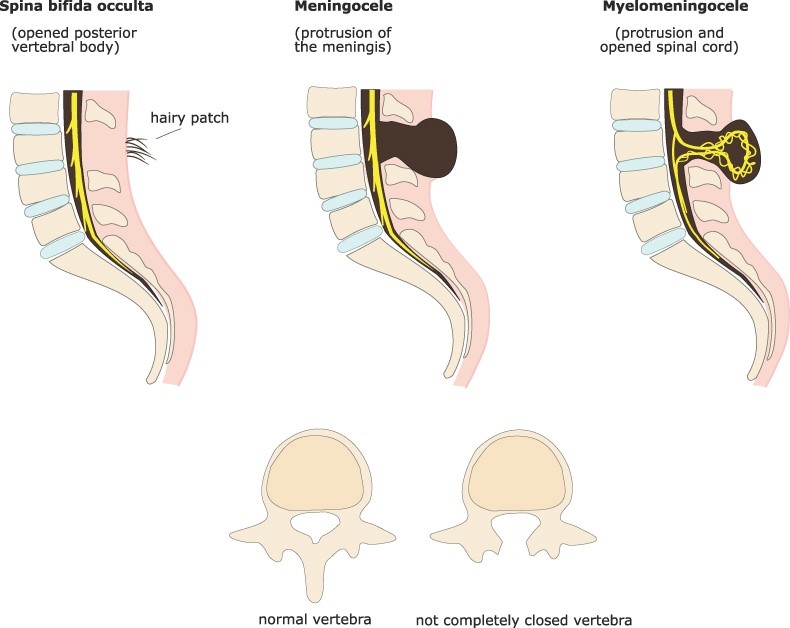
Spina bifida Cystica
This type is characterized by presence of the cyst. It could be
- Meningocele – Cystic swelling of the dura and arachnoid [meninges] which protrudes through the defect in the vertebral arch.
- Meningomyelocele – Cord tissue extends into the meningocele. It is the most common type of spina bifida [94% cases of all excluding spina bifida occulta]
- Myelocele or myeloschisis – Severest form of spina bifida cystica where the open neural plate has spread out onto the surface and is covered just by epithelium.
Meningocele
In this condition protrusion of meninges occurs through the defect in the neural arch. Such protrusion contains only cerebrospinal fluid. So it gives rise to cystic swelling.
Usually, the duramater stops at the margin of the defect and usually the pia and arachnoid protrude. The overlying skin remains intact.
It is common in the lumbosacral region. [Meningocele also occurs in the skull in the occipital region or at the root of the nose.]
The meningocele is present since birth and is seen as cystic, highly translucent and compressible swelling. The overlying skin is normal and not adhered.
Neurological manifestations are usually absent in contrast to myelomeningocele.
When associated with hydrocephalus, the condition is known as Arnold-Chiari syndrome.
X-ray is confirmatory and will show the bony defect. Infection and rupture are possible complications
The treatment requires surgical repair which is done within a few days of birth.
Meningomyelocele
Meningomyelocele is the commonest variety of spina bifida in living children. The bony defect in this is large and can extend over 3 or more segments. The sac contains cord as well along with the meninges and overlying skin is atrophic. The skin may be absent in some cases exposing meninges.
These patients always have neurological manifestations including paralysis.
Infants may show the following symptoms
- Lethargy
- Poor feeding
- Irritability
- Stridor [harsh sound while breathing]
- Eye coordination problem.
Older children may present with
- Cognitive changes
- Motor weakness
- Spasticity
- Bladder/bowel symptoms
- Backache
- Deformities of lower limb [see associations]
- or deformities of the lower limb.
- Tethered cord [tissue attachments cause stretching of spinal cord.]
X-ray will show the bony defect. There may be other abnormalities of the vertebrae, like scoliosis or kyphosis or even hemivertebra.
Based on the level of involvement, myelomeningocele patients frequently can be classified as
Thoracic
-
- upper limb and neck musculature well innervated
- Variable function of trunk muscles
- No power in lower limbs.
High lumbar
- Variable hip flexor and hip adductor
- Absence of hip extension, hip abduction,
- Absent knee and ankle movements
- Increased prevalences of
- Lumbar lordosis
- Abduction and external rotation contractures of hip
- Flexion contracture of knee
- Foot equines
Low lumbar
- Present – hip flexors and adductors, medial hamstring, and quadriceps
- Variable – lateral hamstrings, hip abductors, and ankle dorsiflexors
- Absent – Ankle plantar flexors
- Deformities
- Hip and knee flexion contractures
- Increased lumbar lordosis
- Genu valgum [knock knees]
- Calcaneo-valgus and overpronation foot deformities
Sacral
- Hip, knee normal
- Ankle plantar flexor strength is variable.
- Mild hip and knee flexion contractures
- Increased lumbar lordosis
- Variable foot and ankle deformities
Myelomeningocele should be operated at the earliest if condition of the child allows.
Dealy in surgery may increase the risk of
- Infection within the sac
- Sac rupture
- Adhesion of nerves leading to difficulty during surgery
- Gradually extensive paralysis of the legs and incontinence [leading to contraindication of surgery]
Apart primary sac surgery following are additional management issues and modalities
- Bladder and bowel management
- Bracing and orthotics
- Physical and occupational therapy
- Hydrocephalus management
- Chiari malformation repair
- Deformity correction
- Fracture management
Syringomyelocele
The central canal of the spinal cord is dilated and the spinal cord lies within the sac together with the peripheral nerves arising from the cord.
This is the rarest variety of spina bifida.
Gross neurological deficits and paralytic manifestations are present.
Myelocele
This is the gravest form of spina bifida, in which besides the bony defect there is also a defect of development of the spinal cord. The development is arrested before the time of closure of the neural furrow. So that the posterior part of the spinal cord is not developed.
Majority of the cases are stillborn. Even if a few born alive, they die within a few days from infection of the cord and meninges.
Diagnosis of Spina Bifida
Barring occulta, the most common type of spina bifida is myelomeningocele. Spina bifida occulta too has some signs like a tuft of hair, mole, or dimple on the overlying skin.
Most of the following discussion concerns meningomyelocele.*
X-rays can not only confirm the underlying defect but also reveal spinal deformities and any bony changes. X-rays can highlight hip dislocation and other deformities.
MRI is important to look for the change in neurological structures and the presence of tethered cord.
Alpha-fetoprotein (AFP) levels in the second trimester of pregnancy may provide cues to the diagnosis as these are
elevated in 75% of children with open spina bifida.
AFP levels are also used as a screening test in combination with ultrasonography for prenatal diagnosis.
Other diagnostic lab tests in cases of known spina bifida are
- Routine biochemistry examination
- Urine studies for culture
- Urodynamic studies for bladder evaluation
- Latex sensitivity [It is commonly seen among these patients] tests
CT is useful for tracking hydrocephalus.
Management of Spina Bifida
People with spina bifida occulta may not need any treatment at all unless there is a cosmetic issue of tuft of hair or lipoma. Rarely intradural lipomas can cause compression of the surrounding structures and need to be removed.
The persons with meningocele or myelomeningocele will almost certainly need to repair their spinal defect.
The surgery aims to repair the spinal defects but it is just part of the management and a curative procedure.
The surgery is increasingly performed in the prenatal [before birth] period too. The surgery is performed before 26 weeks of pregnancy. Some studies have suggested that repairs before birth are associated with less disablity.
It must be noted that prenatal surgeries are associated with potential procedural risks to both child and mother. So patient selection needs to be done carefully.
Postnatal surgeries are performed when the child is one or two days old.
The nerves are pushed back into the spinal canal and gently covered with skin and muscles. Any tissue trapped issues trapped in the myelomeningocele is freed.
Other procedures that may be of the need for the complications are
- Surgery for hydrocephalus
- Tendon release in limb
- Repair of spinal deformities
- Posterior fossa decompression to relieve fluid buildup on brain
- Release of tethered spinal cord
- Repair of bladder or bowel problems
Complications of Spina Bifida
The severity of complications varies with the severity of spina bifida present. Following are common complications that are encountered in spina bifida patients
- Poor Bowel and Bladder Control
- Prolonged catheterization
- Self catheterization in later life
- Hydrocephalus – Increased fluid buildup in the brain
- Most people require shunt surgeries
- Chiari malformation need repair
- Latex Allergy
- Often due to latex exposure due to prolonged catheterization and frequent surgeries
- Use of latex-free products can help
- Limited mobility
- May need mobility aids [braces, crutches, wheelchair] depending on the severity
- Deformities of spine and limb
- Physical therapy and deformity correction
- Skin Issues
- Frequent ulcers may occur where the region is numb
- Prevention and treatment by padding adequately and frequent skin care helps
- Sleep Apnea
- Tethered Spinal Cord
Prevention of Spina Bifida
Increased use and accuracy of prenatal diagnosis and option for early pregnancy termination and the introduction of primary prevention in the form of folic acid therapy has resulted in a decline of cases of spina bifida.