Last Updated on October 28, 2023
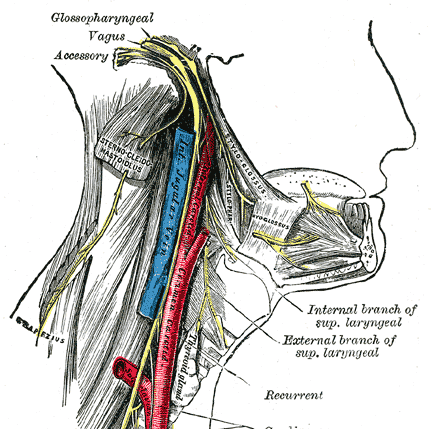
The spinal accessory nerve [ also called accessory nerve] is eleventh cranial nerve (CN XI) [see the controversy below] and is composed of two parts, the cranial part, and the spinal part. It has a purely somatic motor function, innervating the sternocleidomastoid and trapezius muscles.
The sternocleidomastoid is a neck muscle that tilts and rotates the head whereas trapezius is a back muscle that is inserted on to the scapula, acts to shrug the shoulder.
There are 12 pairs of cranial nerves in total which are numbered using Roman numerals I – XII. The spinal accessory nerve is also called cranial nerve XI.
Why It is Called Spinal Accessory Nerve
The spinal accessory nerve used to be called the accessory nerve (XI) because it is a combination of 4-5 little rootlets from the medulla and 5-6 rootlets from the first five cervical vertebrae. These rootlets merge into one bundle that goes to the base of your brain stem.
It was later found that the spinal accessory nerve actually loses its cranial nerve rootlets to the vagus nerve which is the tenth cranial nerve and is located just above it.
Thus spinal accessory nerve’s cranial component actually belong to the vagus nerve. As a result, the nerve bundle name was changed to the spinal accessory nerve, reflecting the fact that this nerve only controls functions of the spinal branch.
There is an ongoing debate about whether the cranial part should be considered part of the accessory nerve proper or not
Still, the term accessory nerve is used interchangeably.
Origin and Course of Spinal Accessory Nerve
The spinal accessory nerve is the only cranial nerve to both enter and exit the skull.
The spinal accessory nerve is formed by 2 parts.
- Spinal
- Cranial
The spinal or motor part is formed by the fibers that originate in the ventral horn of the upper 4 or more [sometimes up to 7] cervical segments of the spinal cord. These fibers join together to form rootlets, roots, and finally the nerve bundle.
The cluster of neurons from where spinal fibers origin, called the spinal accessory nucleus, is located in the lateral aspect of the anterior horn of the spinal cord.
This nucleus stretches from spinal cord junction with the medulla through to the level of about C6.
[It is interesting to note that the lateral horn of high cervical segments seems continuous with the nucleus ambiguus of the medulla oblongata. Cranial component of spinal accessory nerve originates from nucleus ambiguus.]
The spinal fibers ascend lateral and parallel to the spinal cord and enter the cranium through the foramen magnum.
These fibers are joined by second part [accessory or cranial component] of the spinal accessory nerve that originates in the nucleus ambiguous in the medulla oblongata. The cranial part (accessory portion) is the smaller of the two.
It runs laterally to the jugular foramen, where it interchanges fibers with the spinal portion or becomes united to it for a short distance. A recent study has refuted any connection between the spinal and cranial component and claims that both nerves are surrounded by a distinct sheath in the majority of the cases.
After the two components join, the bundle traverses the posterior cranial fossa to reach the jugular foramen. The nerve leaves the skull through the jugular foramen in the same dural compartment as the vagus nerve. After passing jugular foramen, the nerve divides variably into the two original components.
The superior branch containing accessory or cranial component joins the vagus nerve either directly or through the ganglion nodosum and then contributes to the pharyngeal, laryngeal, and cardiac sympathetic fibers.
[Most consider the cranial part of the eleventh cranial nerve to be functionally part of the vagus nerve.]
Thus after leaving the skull, the cranial component detaches from the spinal component.
The other nerve, also known as spinal or lateral branch continues alone and heads backward and downwards. It is essentially a pure motor nerve that innervates the sternocleidomastoid and trapezius muscles.
It passes beneath the posterior belly of the digastrics muscle and the upper end of the sternocleidomastoid muscle along the internal jugular vein. It may travel either anterior or posterior to the occipital artery.
It may connect with the second cervical nerve before entering the sternocleidomastoid.
The nerve emerges from the posterior border of the sternocleidomastoid muscle and obliquely crosses the posterior cervical triangle downward to enter the trapezius muscle.
The extracranial course of the accessory nerve is relatively superficial (it runs between the investing and prevertebral layers of fascia), and thus vulnerable to damage. [Iatrogenic injuries is the most common cause of injury to this nerve.]
Various and variable connections to the spinal accessory nerve are from greater auricular nerve (C2, C3), cervical roots (C2, C3, C4), phrenic nerve and brachial plexus
In the posterior neck, the spinal accessory has a superficial and variable course beneath the superficial cervical fascia embedded in fibrofatty tissue and is found in relation to a group of 5-10 superficial nodes.
Beneath the trapezius, it forms a plexus with the third and fourth cervical nerves, and from this plexus, fibers are distributed to the muscle. But it also has a single branch that runs to the upper trapezius without any communication with cervical nerves. It provides independent innervation to the upper muscle fibers of the trapezius.
Landmarks for Location
As most of the injuries to this nerve are caused by iatrogenic reasons, it is important to know the landmarks for identification.
Below Mastoid
Enters the deep surface of the sternocleidomastoid muscle 4cm or more below the mastoid process.
Greater Auricular Nerve
The greater auricular nerve has been used as a landmark to identify the spinal accessory nerve as it emerges from the posterior margin of the sternocleidomastoid muscle. The spinal accessory nerve is always found above the greater auricular nerve within a distance of 10.7 mm, with a standard deviation of 6.3 mm.
Lateral Neck
Where it disappears under the deep surface of the trapezius muscle, roughly two fingerbreadths superior to the clavicle at the anterior margin of the trapezius muscle.
Clavicle
The spinal accessory nerve can be identified approximately 51.3 mm with a standard deviation of 17 mm) above the clavicle as it enters the anterior border of the trapezius. This is a constant landmark and is often helpful in identifying the distal end of the nerve.
Trapezius
The superficial cervical vein is a branch of the external jugular vein vascularizes the anterior margin of the trapezius muscle close to the site at which the main trunk of the SAN innervates the trapezius muscle.
Surface Anatomy
Draw a line from the angle of the mandible to the tip of the mastoid process. Make another line bisecting this at a right angle. Extend the second line downward across the posterior triangle to get the course of the accessory nerve.
Functions of Spinal Accessory Nerve
Spinal accessory nerve supplies sternocleidomastoid and trapezius muscles
Sternocleidomastoid
This is a muscle that gets taut when we turn neck. It is attached to the sternum and clavicle on one side and mastoid process on the other.
It causes lateral flexion and rotation of the neck when acting unilaterally. The bilateral action causes extension of the neck at the atlanto-occipital joints.
Trapezius
The trapezius is a big muscle that originates from the base of the skull and the spinous processes of the C7-T12 vertebrae to lateral third of the clavicle. It attaches to the acromion of the scapula.
It is made up of upper, middle and lower fibers.
- The upper fibers of the trapezius elevate the scapula and rotate it during abduction of the arm.
- The middle fibers retract the scapula
- The lower fibers pull the scapula inferiorly.
Clinical Significance
Accessory spinal nerve palsy can lead to paralysis of sternocleidomastoid and trapezius.
The most common cause is an iatrogenic injury during surgery. The superficial and variable course of the nerve in the neck makes it vulnerable.
The nerve function is examined by asking the patient to rotate their head and shrug their shoulders, both normally and against resistance.
Other clinical features include muscle wasting of the muscles.