Last Updated on October 29, 2023
Blount disease, also termed as tibia vara is characterized by disordered endochondral ossification of the medial part of the proximal tibial physis. Though it is called tibia vara, actual deformities are multiplanar – tibia with varus, procurvatum (a deformity where the apex of angulation is anterior), and internal rotation. It is named after Walter Putnam Blount, an American pediatric surgeon.
Blount disease can lead to a progressive deformity with gait problems, limb-length discrepancy, and early degenerative arthritis of the knee. Deformities of the distal femur may also be present. A predisposition for obese black children and children of Scandinavian descent has been noted.
Types of Blount Disease
There are mainly two types of Blount disease
- Early-onset or infantile – Limb deformity develops before age of 4 years
- Late-onset – Limb deformity develops after the age of four years.
Late-onset Blount disease is further divided into juvenile type (4-10 years) and an adolescent type (>10 years).
Bilateral involvement is common in Blount disease, particularly with an early-onset presentation.
Langenskiold Classification of Blount disease
Langenskiold in 1952 described six progressive stages visible MRI stages for the infantile type of Blount disease. This classification is based on different degrees of epiphyseal depression and metaphyseal fragmentation of the proximal medial tibial epiphysis.

Stage I
Medio-distal beaking of the upper proximal tibial metaphysis.
Stage II
Wedging of the medial part of the upper tibial epiphyseal secondary ossification center plus a saucer-shaped defect of the upper surface of the metaphyseal beak due to its dissolution, fragmentation & collapse.
Stage III
Stepping of the infero-medial border of the secondary ossification center but without extending distally to the physeal plate level plus deepening of the metaphyseal saucer into a step in the medial metaphysis.
Stage IV
The epiphyseal secondary ossification center passes more distally and crosses distal to the physeal level to fill the metaphyseal step.
Stage V
Separation of the most medial part of the ossification center from the bulk of the secondary ossification center and resides now in the depth of the metaphyseal step below the physis. This is radiologically expressed as either a horizontal cleft (double epiphysis) or complete absence of the medial secondary ossification center as it will be overshadowed by the upper medial tibial metaphysis.
Stage VI
Medial epiphyseal plate closure with a bony bridge.
Etiology and Pathogenesis
The cause of Blount disease is not known and a combination of hereditary and developmental factors has been suggested. It has been found that Blount disease occurs more in children who start walking at an early age and those who are overweight. Therefore, mechanical causes have been suggested to be responsible. The excessive mechanical force at the medial portion of the proximal tibial epiphysis which is still cartilaginous leads to change in the structure and function of the chondrocytes and delayed ossification of the epiphysis.
An obese child with large thighs cannot adduct the hips properly and this produces a varus moment on the knees [fat-thigh gait] thus increasing pressure at the medial part of the proximal tibial physis.
Childhood obesity has also been found to reduce bone mineral content which may further predispose to the development of progressive deformities with increasing weight.
However, mechanical theory alone cannot explain the occurrence of disease only on one side or asymmetrical severity. Therefore, it is suggested that Blount disease may have a genetic predisposition as well.
Many authors believe that disease progression is the result of this cycle of growth disturbance, varus deformity, and further growth disturbance.
Presentation of Blount Disease
Early onset disease presents with varus deformity of the tibia and internal tibial torsion. The disease is usually present on both sides.
In early Blount disease, distinguishing the disease from physiologic bowing, though difficult, is important as varus knees is a very common finding in these children.
Children generally do not report pain, although they can present with a significant deformity. The metaphyseal prominence, or beak, may be palpable over the medial aspect of the proximal tibial condyle.
In contrast, patients with adolescent Blount disease often report pain at the medial aspect of the knee. These patients are typically overweight or obese. In contrast to the early-onset form of the disease, involvement is more commonly unilateral and patients also often have abnormalities of the distal femur.
Lab Studies
Laboratory studies have not been shown to aid in the diagnosis of Blount disease.
Imaging
Plain Radiographs
Radiographs of the knee are critical in assessing and staging the severity of the deformity in Blount disease. A standing full-length anteroposterior radiograph of the entire length of both lower extremities with the patellae forward is crucial for a detailed evaluation of the deformity.
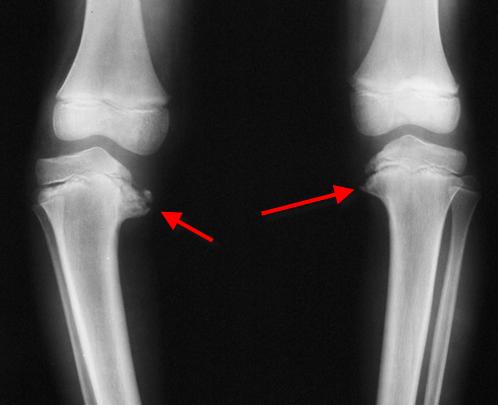
characteristic changes associated with Blount disease include
- Medial beaking of the epiphysis
- Widened irregular medial physis
- Sharp varus angulation of the metaphysis
- Irregular ossification
- Medial slope of the epiphysis and metaphysis in varus.
In addition to the Langenskiöld classification, the following measurements are used to differentiate Blount disease from physiologic tibia vara.
Tibiofemoral Angle
The angle between a line drawn from the center of the hip to the center of the knee and a line drawn from the center of the knee to the center of the ankle. The severity of the varus deformity is based on the tibiofemoral angle as measured on standing hip-to-ankle anteroposterior radiographs. The metaphyseal-epiphyseal angle is the angle formed by the intersection of a line through the transverse plane of the proximal tibia epiphysis with a line through the transverse plane of the metaphysis.
Metaphyseal-Diaphyseal Angle
The angle between a line drawn through the most distal aspects of the medial and lateral beaks of the proximal tibial metaphysis and a line perpendicular to a line drawn along the lateral aspect of the tibial diaphysis.
- >16 ° is considered abnormal and has a 95% chance of progression
- <10 ° has a 95% chance of natural resolution of the bowing
Femoral Metaphyseal-Diaphyseal Angle
The angle between a line drawn perpendicular to the anatomic axis of the femur and a line drawn parallel to the distal femoral physis.
Epiphyseal Metaphyseal Angle
The angle between a line drawn through the proximal tibial physis, parallel to the base of the epiphyseal ossification center, and a line connecting the midpoint of the base of the epiphyseal ossification center with the most distal point on the medial beak of the proximal tibial metaphysis.
Percentage Deformity of Tibia
The percentage deformity of the tibia is calculated as the degree of tibial varus (the medial angle between the mechanical axis of the tibia and a line drawn parallel to the distal femoral condyles) divided by the total amount of limb varus (femoral varus [FV] + tibial varus [TV]). Femoral varus is represented by the medial angle between the mechanical axis of the femur and a line parallel to the distal femoral condyles.
In adolescents, approximately one-third of the varus deformity in adolescents with late-onset disease may be attributable to the distal part of the femur.
MRI
MRI can define intra-articular changes such as posteromedial depression of the tibial plateau and hypertrophy of the medial meniscus in children with early-onset disease. Growth plate irregularities and early physeal bar formation can also be determined.
CT
CT with 3-D reconstructions is useful for preoperative planning in children with early-onset Blount disease presenting with recurrent deformities
Treatment of Blount Disease
Options for treatment of Blount disease include orthoses and surgery. If infantile Blount disease is diagnosed before age 4 years, non-operative treatment in form of orthoses has a role in Langenskiöld stage I or II diseases, especially with unilateral involvement.
In late-onset patients and early-onset patients in whom brace management fails, operative intervention is indicated.
Surgical options available are corrective osteotomy, lateral hemiepiphyseodesis, and guided growth around the knee, gradual asymmetrical proximal tibial physeal distraction, resection of a physeal bar, and elevation of the medial tibial plateau.
Orthoses
Knee-ankle-foot orthoses with a medial upright and drop-lock hinges in children younger than thirty-six months of age with early-stage (Langenskiold stage I or II) Blount disease.
Bracing must continue for approximately 2 years for resolution of bony changes though if successful, improvement is visible within 1 year. Outcome improves if the condition is unilateral.
Obesity with a weight greater than the 90th percentile, varus thrust, an age older than three years at the initiation of the brace treatment, bilateral involvement, and Langenskiöld stage-III or higher disease puts the treatment into a higher risk of failure.
Operative Management
Surgery is contraindicated in children < 2 years because it is difficult at this age to differentiate between Blount disease and physiologic bowing. Surgical outcomes are better if surgery is performed before 4 years of age.
Hemiepiphyseodesis
Hemiepiphyseodesis involves fusion of the lateral aspect of the proximal part of the tibia and relies on the growth of the remaining healthy part of the physis for angular correction.
Guided Growth
This procedure aims to correct further growth at the growth plate. Small metal plates are secured to the bone across the healthy side of the growth plate to halt the growth on that side of the tibia, which enables the affected, abnormal side of the growth plate to catch up, and therefore correct the deformity.
Both hemiepiphyseodesis and guided-growth systems are safe options but do not address limb shortening. These options may be considered for adolescents who have <15° of varus deformity, have at least two years of skeletal growth remaining, and have no more than 1 cm of limb shortening
Proximal Tibial Metaphyseal Osteotomy
Osteotomy can aim for acute correction or gradual correction.
Acute correction of angular and rotational deformity in Blount disease can be accomplished with a proximal tibial metaphyseal osteotomy. The type of osteotomy [closing wedge, opening wedge, dome, serrated, and inclined osteotomies] and type of fixation methods [cast immobilization, k-wires, interfragmentary screws, plates and screws, external fixators] depend on the patient’s age, body habitus, the deformity, associated sagittal and axial plane deformities, and the surgeon’s experience.
There is a potential for neurologic injury and compartment syndrome with acute correction.
Osteotomy with gradual correction employ the use of special external fixators like Taylor spatial frame and employ the principle of distraction osteogenesis. It is a safe and effective method with a lesser incidence of complications like neurovascular injury and compartment syndrome. Pin-site infection is a problem.
Asymmetrical Physeal Distraction
This method is used in adolescent patients and involves placing two 6-mm half-pins were placed into the proximal tibial epiphysis and two pins were placed into the diaphysis and gradual distraction without fibular osteotomy leading to angular correction of the deformity.
This method leads to premature closure of physis.
Physeal Bar Resection
This has been tried in children with advanced stages of early-onset Blount disease and involves resection of a physeal bar at the medial aspect of the proximal part of the tibia with interposition of fat or silicone and a simultaneous valgus osteotomy. Long-term follow up is not available
Elevation of the Medial Plateau
Elevation of the medial tibial plateau is recommended for the few children older than six years of age with Langenskiöld stage V or VI Blount disease and substantial posterior depression of the medial tibial plateau.
Prognosis
Infantile Blount disease has a good prognosis, and early treatment is associated with low recurrence.
Untreated infantile tibia vara is believed to be progressive though partial or complete regression is known in the early stages of the disease. However, later stages continue to progress and eventually lead to joint degeneration.
In the late-onset form of the disease, regression does not occur and the varus deformity may worsen over time.