Last Updated on February 28, 2020
The term chondroma refers to a benign tumor of cartilage origin. The tumor contains cartilage cells that are similar to normal cartilage cells but contains vessels that differentiate it from normal cartilage.
Chondromas may arise inside or outside the bone. These tumors are called enchondromas when they occur in the medullary canal of the bone. The one that grows outward from the bone is called ecchondroma but popularly referred to as chondroma only and often prefixed by the site.
Thus they and are called periosteal or juxtacortical chondromas when they occur on the surface of the bone.
These can also arise from the synovial sheath are called synovial chondromas.
The lesions can occur in soft tissue like tendons of hand and feet where they are called extraskeletal or soft tissue chondromas. These are very rare.
Enchondromas are most common chondromas and 3-10% of all bone tumors. Periosteal chondromas are rarer and account only for 1% of all chondromas
No age preponderance is seen though incidence peaks in the third and fourth decades.
Enchondromas do not show any sex predilection but periosteal chondromas occur more commonly in male individuals
Pathophysiology
Chondromas develop from nests of growth-plate cartilage that have become entrapped in the medullary canal of the metaphysis or in the metaphyseal-diaphyseal junction. These are hamartomatous proliferations that persist as islands in the bone and then develop from enchondral ossification.
They respond to the same growth factors as normal cartilage and grow until adulthood.
Chromosomal abnormalities involving the 12q13-q15 chromosomal region may be associated with chondroma, especially soft-tissue chondroma.
Periosteal chondroma tends to develop within and beneath the connective tissue of periosteum.
Synovial chondroma results from cartilage metaplasia of subsynovial connective tissue.
Clinical Presentation
Enchondroma
Two-thirds of the lesions occur in small bones of hand and feet. Long tubular bones are affected next femur, proximal humerus being most common.
Metaphyses are more commonly affected than diaphysis.
Flat bones like pelvis, ribs, scapulae, and vertebrae are rarely affected.
Most of the enchondromas do not lead to symptoms and are diagnosed on x-rays as an incidental finding.
When enchondroma involves short tubular bones of the hands, it can result in bulbous swelling of the fingers.
Pain is often not present. A complaint of pain should raise the suspicion of microfracture or a malignant transformation.
Enchondromatosis is a condition where there are multiple enchondromas typically metaphyseal commonly affecting appendicular skeleton. The condition is pathologically different from benign enchondromas and the cartilage has a propensity for continuous slow growth. These lesions carry a higher risk of secondary sarcomatous change.
Ollier disease is the most common type of enchondromatosis.
When enchondromatosis is associated with soft-tissue hemangiomas of skin, soft tissues, and visceral organs, it is called Maffucci syndrome.
Periosteal chondroma
Periosteal chondromas typically involve long bones, proximal humerus being most common. Short tubular bones can also be affected.
They are usually metaphyseal lesions but can occur in diaphyseal sites as well.
These chondromas occur on the surface of the bone and present as palpable swellings.
They are otherwise painless but may interfere with the function of these tendons and other structures leading to pain during motion of the joint.
Soft-tissue chondroma
Soft-tissue chondromas tenosynovial sheaths or soft tissues adjacent to tendons in the hands and feet of adults. from chondrosarcomas.
Synovial chondromas can be diffuse [multiple nodules all over synovium] or localized [descrete mass].
In the rare nodular variety of synovial chondromatosis, a polypoidal pedunculated mass protruding into the joint may also be a feature. The large cartilaginous masses have multinodular granular surfaces, and individual nodules may range in size from less than 1 mm to 1-2 cm.
Extraskeletal chondromas are occurrence but have been reported in hands, feet, nasal tip, scalp, palate.
Soft tissue chondromas are known to undergo secondary changes like including dystrophic calcification, enchondral ossification, myxoid degeneration, and hemorrhage in the lesion which make them difficult to differentiate from chondrosarcoma.
Lab Studies
These do not help in diagnosis per se. Routine investigations are
X-ray
Enchondroma
- Localized radiolucent defect
- Usually, metaphyseal in long bones
- Diaphyseal in short tubular bones but may extend to the epiphysis
- Variable punctate or stippled calcifications
- Short tubular bones may be expanded
- Usually cortices intact
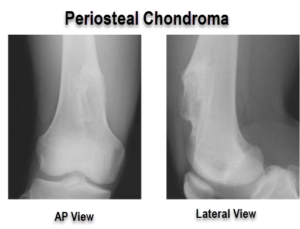
Periosteal chondroma
- Well-defined surface lesion with stippled or punctate calcifications
- Underlying cortex may get eroded
- Subchondral sclerosis in long-standing tumors
- Elevation of the periosteum that overlies the lesion forming, this finding appears as solid buttresses subperiosteal bone.
CT
CT enables to visualize subtle changes such as change in calcification and can lead to early identification of malignant transformation.
(PET)-CT [Positron emission tomography] is better at differentiating chondroma from intraosseous chondrosarcoma in long bones.
MRI
MRI can be used for assessment of
- Noncalcified intramedullary chondroid lesions
- Any local extension [spread is seen in chondrosarcoma but not in chondroma]
Biopsy
If the lesion is clinically and radiologically benign, a biopsy is not needed.
The biopsy is done in case of doubtful diagnosis.
Grossly, enchondromas are small lobules with irregular periphery with or without satellite lesions.
Cross section appears ivory white because of calcification.
Periosteal chondromas are as lobulated, cartilaginous covered with fibrous tissue. The cortex might be scalloped and thickened.
Microscopic findings are that of lobules of mature hyaline cartilage with varying cellularity. Areas of myxoid change or focal necrosis may be seen.
Fine or coarse calcifications and areas of enchondral ossification may be visible.
Treatment
Enchondroma
In long bones, enchondromas are often not symptomatic. Therefore, no treatment is needed in most of the lesions.
For painful lesions and lesions where the diagnosis is not definite, curettage may be done. The tissue removed is subjected to histopathological examination. If it is enchondroma, nothing further needs to be done.
If the lesion comes out to be malignant, further workup and treatment is desired.
Patients with pathologic fractures with chondromas would require fixation. The lesion may be curetted at the time of surgery.
Short tubular bones get deformed with enchondromas and often are treated with curettage and bone grafting.
Enchondromas of axial skeleton [rare] are always treated with wide local resection. This is because enchondromas look like low-grade chondrosarcoma and can often not be differentiated. Secondly, the axial skeleton is more common site for chondrosarcoma than enchondroma.
Tissue removed should be subjected to histopathological examination.
Recurrence of the lesion should also raise the suspicion of malignancy.
Recurrence is more common in tubular bones especially in multiple enchondromas but malignant transformation is rare.
Periosteal chondroma
Wide local excision is a curative procedure for this lesion
Synovial chondroma
Synovial chondroma is a local self-limiting condition and may reach a quiescent stage. Depending on the symptoms (especially if they are only mechanical), removal of loose bodies may be all that is required. However, if the lesion produces frequent symptoms, synovectomy may be needed to control the disease. Frequent recurrences with short intervening periods should raise the suspicion of synovial chondrosarcoma.
Long-Term Monitoring and risk of Malignancy
There is a risk of malignant transformation associated with chondromas especially in patients with enchondromatosis [Ollier or Maffucci syndrome].
Patients should be educated about the warning signs of malignant transformation which are
- Deep dull ache
- Night pain
- Increase in size of the swelling
X-rays obtained at regular follow-ups should be looked for any differences in the radiologic appearance of the lesion than previous x-rays.
Look for
- Change in shape of the lesion
- Increase in size of the lesion
- Change in lucency
- Decrease of calcification
- Recurrence of a lytic lesion in a grafted area suggests malignancy
- Break in the cortex
- Esp in short tubular bones where the lesion causes bone expansion
- Increase in radiolucency of a calcified lesion [indicates active dividing cartilage]
Patients with Ollier disease or Maffucci syndrome need more rigorous follow up than simple benign chondroma.
References
- Lubahn JD, Bachoura A. Enchondroma of the Hand: Evaluation and Management. J Am Acad Orthop Surg. 2016 Sep. 24 (9):625-33. .
- Lewis MM, Kenan S, Yabut SM, et al. Periosteal chondroma. A report of ten cases and review of the literature. Clin Orthop Relat Res. 1990 Jul. (256):185-92.
- Nojima T, Unni KK, McLeod RA, Pritchard DJ. Periosteal chondroma and periosteal chondrosarcoma. Am J Surg Pathol. 1985 Sep. 9(9):666-77.
- Bachoura A, Rice IS, Lubahn AR, Lubahn JD. The surgical management of hand enchondroma without postcurettage void augmentation: authors’ experience and a systematic review. Hand (N Y). 2015 Sep. 10 (3):461-71.