Last Updated on November 12, 2019
Distal femur fractures have traditionally been associated with young patients but are increasing in the geriatric population. They are commonly found in young, healthy males and elderly osteopenic females. With increased use of prostheses, periprosthetic fractures becoming more common
These fractures require anatomically stable fixation.
The fractures represent high energy injury in young patients whereas are low energy injuries in old people.

Anatomy of Distal Femur
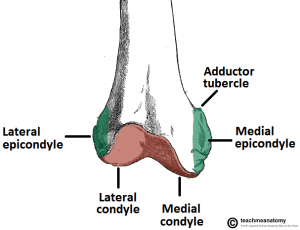
The distal femur is the area where the stronger diaphyseal bone meets the thinner and weaker metaphyseal bone.
The anatomical axis of the knee joint does not coincide with the weight-bearing axis which crosses the center of the femoral head and the center of the knee. The anatomical axis is in valgus and subtends an angle of 81° with the knee joint.
The distal femur, when viewed in cross-section, is seen to be a trapezoid. Anteriorly, the distance between the medial and lateral wall is less than the distance posteriorly. The medial wall has the greater slope of the two and is inclined at 25° to the vertical.
The projected width of the femur on a radiograph is the maximum width and represents the most posterior distance between the medial and lateral wall.
Medial condyle extends more distal than lateral condyle. Posterior halves of both condyles are posterior to posterior cortex of femoral shaft.
Different muscles attached to the condylar area cause different deformities of the distal fragment.
- Gastrocnemius: extends distal fragment (apex posterior)
- Hamstring and extensor mechanism: cause shortening by pulling proximally
- Adductor magnus: leads to distal femoral varus
Read more on Anatomy of Femur
Classification of Distal Femur Fractures [AO/ASIF]
-
A – Extra-articular [Supracondylar Fractures]
- A1 – Simple
- A2 – Metaphyseal, wedge
- A3 – Metaphyseal, complex
-
B – Partial articular
- B1 – Lateral condyle (sagittal fracture line)
- B2 – Medial condyle (sagittal fracture line)
- B3 – Frontal (coronal fracture line) {Hoffa’s fracture}
-
C – Complete articular
- C1 – Articular and metaphyseal segments, simple fractures
- C2 – Articular simple, but metaphyseal multifragmentary fractures
- C3 – Articular and metaphyseal segments, multi-fragmentary fractures
Clinical Presentation
Patients present with pain, deformity, weakness, and inability to use the leg. Young patients often sustain high energy trauma and elderly patients usually have a history of a fall.
The patient needs to evaluated for skin integrity, vascular status in the affected limb.
Full trauma evaluation is warranted if the injury is due to a high energy mechanism.
Any fractures in other areas must be identified. High alert is required for the identification of compartment syndrome.
Imaging Studies
X-rays
Patients with Distal femur fractures require anteroposterior and lateral. Anteroposterior, lateral, and oblique traction views can help characterize injury but are painful
Elderly patients should be evaluated for the degenerative joint disease.
Suspected injuries in the same limb or other body parts should be evaluated.
CT
CT scan is very useful in intra-articular fractures. It helps to
- Identify intra-articular fractures in both frontal and sagittal reconstructions.
- Establishing intra-articular involvement where x-ray does not clearly tell
- Identification of separate osteochondral fragments in the area of the intercondylar notch
- Identification of Hoffa’s fracture which can be easily missed on x-rays.
Angiography
Indicated in suspected arterial injury and associated knee dislocation.
Treatment of Distal Femur Fractures
Essentially all distal femur fractures require operative intervention because of the severe potential risks of prolonged bed rest.
Patients who are bedridden or nonambulatory with nondisplaced or minimally displaced fractures may not be candidate for surgery.
Patients with severe life-threatening or other medical problems in which the risks of anesthesia are high may also be treated nonoperatively.
These patients can be treated with plaster immobilization followed by a hinged knee brace.
Surgery
If the fracture is open or if there is an associated vascular injury, the patient needs to be operated on immediately. The limb should be splinted while the patient awaits surgery.
Goals in the treatment of all intra-articular fractures are
- Accurate anatomical reduction
- Absolutely stable fixation
- Atraumatic reduction,
- Stable reduction of the metaphyseal component
- Early motion
Indications for surgery
Absolute indications
- Unicondylar Fracture
- Fracture in the coronal plane [Hoffa fracture]
- Open Intra-articular Fractures
- Associated Neurovascular Injuries
- Ipsilateral Fracture of the tibial Plateau or patellar Fracture
- Ipsilateral Fracture of the Tibia (The Floating Knee)
- Multiple Injuries
- Pathological Fractures
Different types of fixations
External fixation
- Usually, a temporary measure until soft tissues permit internal fixation, or until the patient is stable
- Pin placement should be avoided in the area of planned plate placement
Open reduction internal fixation

Open reduction and internal fixation are used in displaced, intra-articular fractures and nonunion.
It provides an anatomic reduction of joint and stable fixation of the articular component to shaft to permit early motion.
Implant choice may vary with the fracture.
- For extra-articular distal femur fractures (A1, A2, A3) or those with condylar fragmentation (C1, C2) –
- Dynamic condylar screw
- Condylar blade plates
- For condylar fractures (B1, B2, B3), a 4.5-mm
- T buttress plate with or without lag screw fixation
- Condylar buttress plate for very distal fractures
- Distal Femoral plates
-
- Bridge plating
- Minimally invasive plating
- Specially designed periarticular plates
- Fixed-angle screw plates


Closed/open reduction and Retrograde IM Nailing
This is a good option for good for supracondylar fractures without significant comminution. It is also a preferred implant in osteoporotic bone,
Distal femur nails also necessitate restoration of the condyles before nail placement.
Distal femoral Replacement
This is used in unreconstructable fracture or fracture with prior total knee arthroplasty with loose component
Postoperative physical therapy is usually required.
Patients need to be monitored until the bone is healed.
Approaches to Knee in Distal Femur Fractures
Anterolateral Approach
- Articular fractures
- For minimally invasive plate osteosynthesis
Lateral parapatellar
- Complex articular fractures
- For Hoffa fracture
Medial parapatellar
Complex medial femoral condyle fractures
Posterior
- Very posterior Hoffa fragment fixation
- Midline incision over popliteal fossa
Complications
Complications of Distal femur fractures include the following:
- Nonunion
- Hardware irritation
- Malunions
- Infection
- Implant Failure
Prognosis
With stable fixation and anatomic alignment leading to intra-articular congruency, most patients do well. Severely comminuted fractures, poor bone quality, poor reduction, and poor fixation worsen the prognosis.
Type C3 fractures are expected to develop significant secondary degenerative changes.
Open fractures have a worse prognosis.
References
- Yang RS, Liu HC, Liu TK. Distal femur fractures of the femur. J Trauma. 1990 Mar. 30(3):315-9.
- Parvizi J, Jain N, Schmidt AH. Periprosthetic knee fractures. J Orthop Trauma. 2008 Oct. 22(9):663-71.
- Yoo JD, Kim NK. Periprosthetic fractures following total knee arthroplasty. Knee Surg Relat Res. 2015 Mar. 27 (1):1-9.
- Schatzker J. Distal femur fractures of the femur. In: Schatzker J, Tile M, eds. The Rationale of Operative Fracture Care. New York, NY:. Springer-Verlag. 1987:255-273.
- Tscherne H. Extra-articular fractures of the distal femur. In: Miller ME, Allgower M, Schneider R, Willenegger H, eds. Manual of Internal Fixation. 3rd ed. New York, NY. Springer-Verlag. 1991:548-51.
- Merchan EC, Maestu PR, Blanco RP. Blade-plating of closed displaced Distal femur fractures of the distal femur with the AO system. J Trauma. 1992 Feb. 32(2):174-8.
- Zehntner MK, Ganz R. Internal fixation of Distal femur fractures after condylar total knee arthroplasty. Clin Orthop. 1993 Aug. (293):219-24.
- Wu CC. Retrograde locked intramedullary nailing for aseptic Distal femur femoral nonunion following failed locked plating. J Orthop Surg (Hong Kong). 2015 Aug. 23 (2):155-9.