Last Updated on October 28, 2023
The long thoracic nerve is a pure motor nerve that arises from anterior or ventral roots of C5, C6, and C7 and supplies serratus anterior muscle. Serratus anterior muscle is responsible for stabilization and protraction movement of the scapula.
It is also called posterior thoracic nerve and the external respiratory nerve of Bell, after Sir Charles Bell who provided its first description.
Origin and Course
Long thoracic nerve arises from the anterior rami of three spinal nerve roots: the fifth, sixth, and seventh cervical nerves (C5-C7).
Sometimes, the root from C7 may be absent. Sometimes, there may be a contribution from the C4 root.
The roots from C5 and C6 pierce through the scalenus medius, while the C7 root passes in front of the muscle.
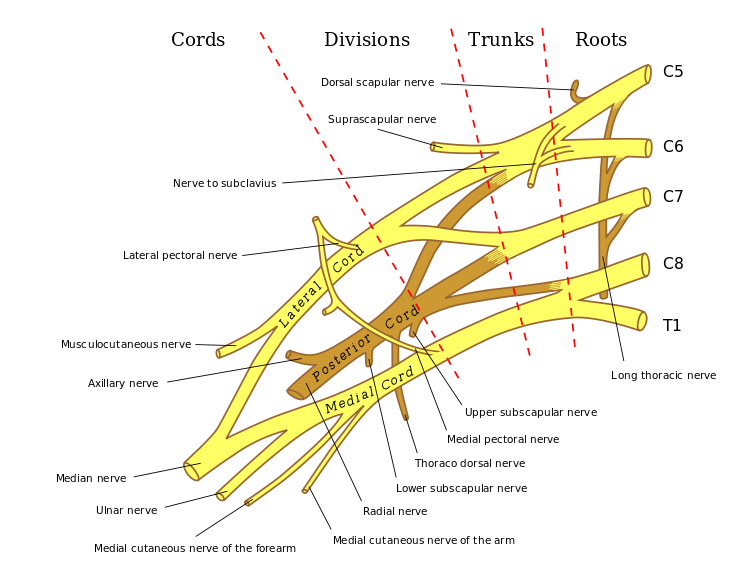
The nerve descends posterior to the roots of the brachial plexus and anterior to the scalenus posterior muscle and has a long course along the chest wall in the mid-axillary line to lie on the superficial surface of the serratus anterior muscle, which it innervates.
The fifth and sixth cervical roots, along with the dorsal scapular nerve, pass through the substance of scalenus medius muscle and join with the root of C7.
The nerve then travels beneath the brachial plexus and clavicle to pass over the first rib. It lies posterior to the first part of the axillary artery.
The nerve descends along the lateral aspect of the chest wall and crosses the outer border of the first rib to reach outer of serratus anterior muscle.
[From its point of appearance to the posterior angle of the second rib, it travels at about 30° posterior angle relative to the anterior axillary line. It then has been noted to pass down between the posterior and middle axillary lines.]
It courses vertically, gets progressively closer to the anterior border of the scapula.
The long thoracic nerve is unique in that it runs superficially to the entire course of the muscle it supplies.
Along with its course over the serratus anterior muscle, the nerve divides into small branches parallel to the main trunk, often several centimeters before turning at right angles and supplying the individual slips by entering the superior aspect of slips.
At the proximal edge of the distal serratus anterior head, it is joined by a collateral branch of the thoracodorsal artery (serratus anterior branch), which crosses over the nerve before dividing into terminal muscle branches. The nerve can be easily identified at this cross-over point, also called Crow’s feet.
Clinical Examination for Long Thoracic Nerve
As the nerve supplies serratus anterior muscle, the examination is done to look for integrity and power of serratus anterior muscle.
The examination involves observation and comparison of both the scapulae and serratus anterior muscles.
Note if there is any the asymmetry between the left and right sides, any atrophy of the muscle, or presence of fasciculations.
Serratus wall test measures and compares the strength of the serratus anterior.
The patient is asked to stand approximately at 2 feet away from the wall, facing it and is asked to push against the wall with the palms flat against the wall at waist level.
Any damage to long thoracic nerve would result in the winging of the scapula due to paralysis of serratus anterior muscle.
Comparison to opposite scapula would help in mild presentations.
Clinical Significance of Long Thoracic nerve
Damage to Long Thoracic Nerve
It may occur for a variety of causes like surgery, trauma to the neck and chest, and sports also result from some sports like archery, tennis etc.
Sports-related nerve damage occurs due to stretching of the nerve. A stretch beyond 10% of the resting length would damage the nerve.
The nerve injury results in serratus anterior paralysis leading to winging of the scapula.
Crow’s foot
It is the point where the long thoracic nerve intersects the most dominant and inferior serratus branch of the thoracodorsal artery
Crow’s foot is an important landmark for flap transfer surgeries.
