Last Updated on November 22, 2023
Osteochondritis dissecans is a condition in which a small segment of articular cartilage with its underlying subchondral bone gradually separates from the surrounding osteocartilaginous tissue due to a lack of blood supply.
Osteochondritis dissecans develops in joints of children and adolescents.
The separation of the fragment may be partial or complete.
The osteochondral segment may always not separate. It may also remain in situ or become partially detached. A fully detached fragment may lodge in the joint as a loose body.
The disease was first described in 1870 by Sir James Paget. The term osteochondritis dissecans was given by Konig.
Osteonecrosis is the condition where the blood supply to a part of the bone stops and the bone dies. The parts of the bone may fragment. However, osteochondritis dissecans occurs in the bone with normal blood supply and this distinguishes it. [An osteoarticular segment becomes avascular rather than a part of the bone].
Two form of osteochondritis dissecans are seen
- Juvenile – occurs in age group 10-15 yea
- Adult- occurs after physis are closed.
The medial femoral condyle of the knee joint is the most commonly involved.
Other locations are capitellum of humerus and talus.
There is a male preponderance.
Causes and Pathophysiology of Osteochondritis Dissecans
The exact cause of osteochondritis dissecans is not known yet. There are various theories that try to explain the causation. There appear multiple factors that have been suggested are
- Injury
- Ischemia
- Genetic factors
Various known risk factors are
- Radiocaptellar joint- Forces that cause valgus stress or compressive forces on radiocpitellar joint
- Repetitive throwing
- Gymnastics
- Weight-bearing on upper extremity
- Talus
- Ankle sprain
- Instability
- Competitive athletics
- Family history
The primary changes take place in the bone. A segment of the bone dies due to lack of blood supply [avascular necrosis of the segment]. This gives rise to the changes in the overlying cartilage.
Initially, the cartilage overlying an area of dissecans appears to be normal, but with loss of subchondral bony support, it undergoes degenerative changes resulting in softening, fibrillation, fissuring of the cartilage. The cartilage loses its sheen also.
Local trauma can cause separation of the subchondral bony fragment.
Healing of the avascular bone occurs by revascularization and repair by creeping substitution. If healing does not occur, a dense fibrous tissue fills the gap.
The pathologic picture invokes both ischemic necrosis and trauma as factors in the pathogenesis of osteochondritis dissecans.
The source of the tissue that fills the defect is the subchondral.
Classification of Osteochondritis Dissecans
The lesion typically progresses through 4 stages in its natural history [Clanton and Lee Classification of Osteochondritis]
Stage I
A small area of compression of subchondral bone.
Stage II
A partially detached osteochondral fragment.
Stage III
A completely detached fragment that remains within the underlying crater bed.
Stage IV
A completely detached fragment that is completely displaced from the crater bed [Loose body]
Clinical Presentation
The usual presenting complaints are
- Intermittent pain in the joint on strenuous physical activity
- Stiffness
- Swelling
- Clicking and locking of the joint
- Limp
The pain of the involved joint is the earliest symptom. Other symptoms appear as the disease gets advanced.
Intermittent symptom-free periods and exacerbation are common.
On examination, the affected leg may be externally rotated during walking. Quadriceps may be found to be weak.
Localized tenderness of area over the lesion may be noted.
Other findings that may be encountered are
- Wasting of muscles
- Synovial thickening
- Swelling of joint
- Limitation of the motion of the joint
- Loose bodies on x-ray
Wilson Test
The patient is in supine or sitting position. The affected knee is flexed to a right angle, the leg is medially rotated fully, and then the knee is gradually extended.
At 30 degrees of flexion, the patient will complain of pain over the anterior aspect of the medial femoral condyle. The pain is relieved on external rotation of the leg.
Imaging
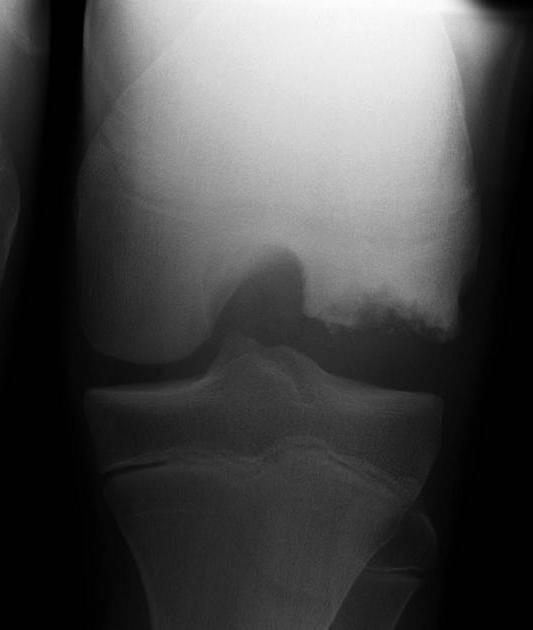
X-rays
Plain x-rays are the first investigation in the evaluation of knee pain.
In osteochondritis dissecans, weight-bearing anteroposterior and lateral views are preferred.
A tunnel or notch view of the knee is obtained by bending the knee between 30 and 50 degrees.
In the early stages, the x-rays are essentially normal and may not be helpful.
The subtle flattening or indistinct radiolucency is the earliest finding on x-rays.
With further advancement of the disease, the following changes are seen
- Changes in contour of the joint surface
- Fragmentation
- Changes in density of the segment
- Well circumscribed fragment of subchondral bone
- Demarcated from the surrounding bone by a radiolucent saucer or crescent-shaped line
- Sclerosis of the affected lesion
As the fragment separates, depression is seen at the site of separation. However, the detached loose body in the joint continues to grow to derive its nutrition from synovial fluid. Osteochondritic fragment becomes radiopaque is due to subchondral bone with articular cartilage, secondary calcification in degenerating articular cartilage and new bone formation following revascularization.
Special views may be necessary to visualize the lesion.
CT
The CT scan makes possible a definitive diagnosis and determines the precise location and true extent of the lesion. It also is able to visualize sectional imaging and thus providing a 3 D perspective. It is ableto differentiate between partial and complete detachment.
MRI
MRI is the imaging of choice for its high sensitivity and specificity. Not only it is able to detect the changes at the earliest but also provides clear visuals of cartilage.
MRI is able to detect instability of the fragment. The classic signs are
- High signal intensity rim between the fragment and the adjacent bone
- Fluid-filled cysts beneath the lesion
- High signal intensity line in the articular cartilage over the lesion
- Fluid filled focal osteochondral defect [Indicates complete detachment]
Bone Scan
This shows localized increased activity at the site of the lesion. It helps to differentiate the lesion from infection.
Management of Osteochondritis Dissecans
Medical Management
In osteochondritis dissecans of the knee, the age and severity of the condition guide the treatment.
Nonoperative treatment consists of
- Restricted weight bearing
- Bracing
This treatment is indicated in
- Stable lesions in children with open physes
- Asymptomatic lesions in adults
50-75% of the lesions will heal without fragmentation.
The bracing is required for about 3 months to allow healing and prevent further displacement.
Normal activity can be allowed to the patient who shows a good response which is gauged by
- Absence of pain
- Normal physical examination
- Radiological evidence of healing.
The patients are followed every 4-6 months until the lesion has healed or until skeletal maturity is achieved.
An asymptomatic patient with nonprogressive radiographic findings needs no further treatment.
Failure of conservative treatment warrants surgery.
Early surgery should be considered in children who are near physeal closure.
Surgical Management
General indications for surgery are
- Inadequate response to nonoperative treatment
- Lesions where skeletal maturity is within 6 months
- Presence of loose bodies
Asymptomatic patients with lesions in weight-bearing joints should be considered for surgery because these lesions may lead to early degenerative joint disease.
All surgical procedures can be done arthroscopically or as open surgery. But arthroscopic surgery is done at an increasing rate now.
Subchondral Drilling
It is done only when the lesion is stable on arthroscopy. Multiple perforations of the lesion are made using Kirschner wires or drill. This leads to the formation of fibrocartilaginous tissue. The procedure has been shown to improve the outcome in the immature skeleton.
Fixation of Fragment
Debridement and fixation of the fragment is done when the lesion is not stable. It has been associated with a >80% healing rate.
A bioresorbable bone fixation nail, bone pegs or a herbert screw can be used for fixation.
Cancellous bone grafting may be required.
Autologous Osteochondral Mosaicplasty
This involves use of cylindrical osteochondral grafts from the minimal weight-bearing periphery to the prepared defects in the affected area.
Autologous Chondrocyte Transplantation
This technique is required for extensive defects in which other treatments have failed.
For this, chondrocytes or cartilage cells are arthroscopically harvested and cultured in a cell culture lab for 2-3 weeks. Cultured cells are injected into the defect, which is covered with a periosteal flap.
Sandwich technique refers to the removal of sclerotic bone, bone grafting and autologous chondrocyte transplantation.
Follow-up
Following arthroscopic subchondral drilling, the affected joint is immobilized until radiological signs of healing are evident.
Then the patient is put on a range of motion exercises.
A similar rehabilitation protocol should be used after fixation with bone pegs.
Following all other surgeries, immobilization is not necessary. Continuous passive motion is administered for 48 hours. Rehabilitation exercises are begun after 48 hours and are continued for 8 weeks. Weight-bearing is gradually introduced into and progressed to full weight bearing by 6-8 weeks.
Prognosis
Juvenile osteochondritis dissecans of a knee, without a loose body lesion, frequently heals with conservative methods.
Adult osteochondritis dissecans, respond better with when surgical intervention.
Different surgeries have a success rate of 70-90%.
References
- Wiesler E, Poehling GG. Osteochondritis dissecans of the capitellum. Tech Shoulder Elbow Surg. 2001. 2:131-8.
- Choi YS, Cohen NA, Potter HG, Mintz DN. Magnetic resonance imaging in the evaluation of osteochondritis dissecans of the patella. Skeletal Radiol. 2007 Oct. 36(10):929-35.
- Michael JW, Wurth A, Eysel P, König DP. Long-term results after operative treatment of osteochondritis dissecans of the knee joint-30 year results. Int Orthop. 2008 Apr. 32(2):217-21.
- Weckström M, Parviainen M, Kiuru MJ, Mattila VM, Pihlajamaki HK. Comparison of bioabsorbable pins and nails in the fixation of adult osteochondritis dissecans fragments of the knee: an outcome of 30 knees. Am J Sports Med. 2007 Sep. 35(9):1467-76. Link