Last Updated on November 19, 2019
Shoulder arthrocentesis is the procedure of aspirating joint fluid from shoulder joint and like other arthrocentesis can have a diagnostic or therapeutic purpose.
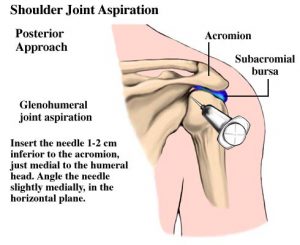
Shoulder joint or the glenohumeral joint can be approached anteriorly or by a posterior approach. The posterior approach allows the patient to be blinded from the procedure, and it mimics the approach used in arthroscopy of the joint.

Indications of Shoulder Arthrocentesis
Diagnosis
- Acute monoarticular [that affects a single joint] arthritis
- Suspected infection (eg, septic arthritis)
- Inflammatory joint effusion
- Gout
- Pseudogout
- Rheumatologic disorders
- Reactive arthropathies
Therapeutic
- To relieve a large painful effusion.
- Instillation of medications
- Repeated arthrocentesis for septic arthritis in carefully selected patients as a means of decreasing bacterial load
Contraindications
- Cellulitis in the overlying skin
- Overlying skin lesions (eg, dermatitis or psoriasis)
- Known bacteremia
- Bleeding disorders
- Patient on anticoagulation medication
Relevant Anatomy
The glenohumeral joint of the shoulder is formed by the humeral head and the glenoid fossa of the scapula.
Detailed anatomy of the shoulder joint
Procedure of Shoulder Arthrocentesis
- Shoulder joint can be approached posteriorly or anteriorly. The patient should be seated in a comfortable position.
- For the anterior approach, the hand of the patient should rest lap so that the shoulder is internally rotated.
- If the posterior approach is contemplated, rest the patient’s hand on the affected side on the contralateral shoulder.
- Palpate and mark the needle insertion site according to the approach chosen
- Anterior approach
- Palpate the coracoid process and the humeral head.
- With the arm in internal rotation [internal rotation is achieved by placing the hand in the lap of the patient.], the joint space can be felt as a groove lateral to the coracoid process.
- Direct the needle slightly laterally and superiorly into the glenohumeral joint space.
- Posterior approach
- The needle is inserted 1-2 cm inferior and medial to the posterior tip of the acromion [and directed anteriorly and medially toward the coracoid]
- Prepare the part according to the entry site chosen. Povidone-iodine and alcohol solution can be used for part preparation. Part preparation is done to sterilize the skin surrounding the insertion site and allow it to dry
- Administer the local anesthesia using 1% or 2% lidocaine.
- The joint is aspirated using 18 gauge or thicker needle. Advance the needle while keeping a pull on the plunger of the syringe until synovial fluid is obtained. The amount if the fluid aspirated would depend on the size of the effusion or intended investigation.
- In case the shoulder is accessed for injection, after aspirating the fluid, stabilize the needle by holding the hub and remove the syringe part and exchange the syringe for a corticosteroid-filled syringe. After the other syringe is in place, the injection can be carried out.
- Remove the needle after the procedure and apply pressure on the site for few minutes. A small sealant bandage can be applied.
- Divide the fluid among the specimen tubes and send for the required investigation.
For increased accuracy of needle placement, ultrasound imaging may be used to locate the size of aspiration.
Complications
Complications are few and rare. These include the following.
- Hematoma
- Intravascular injection into the axillary vessels
- Infection is possible
- Injection of corticosteroids into a tendon or tendon insertion can cause tendon rupture
- Rise in blood glucose levels in patients with diabetes mellitus in case of corticosteroid instillation.