Last Updated on November 19, 2019
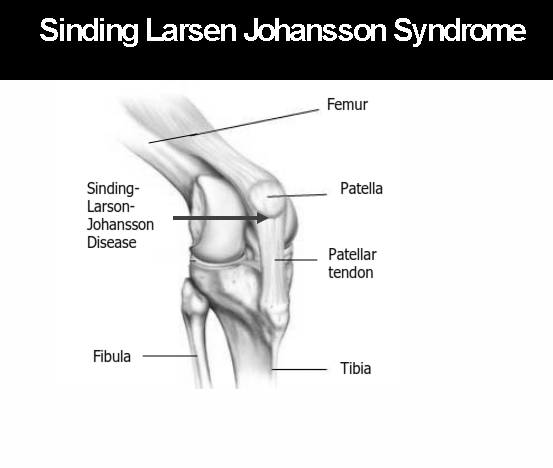
Sinding Larsen Johansson disease [ also known as Sinding-Larsen disease or Larsen-Johannson syndrome] is a type of osteochondrosis that affects the proximal end of the patellar tendon as it inserts into the inferior pole of the patella, and represents a chronic traction injury or overuse injury of the immature osteotendinous junction. It is a closely related condition to Osgood-Schlatter disease. Sinding Larsen Johansson disease is an important cause of anterior knee pain in adolescents.
Sinding Larsen Johansson disease is also called as pediatric Jumper’s knee.
 Both Sinding Larsen Johansson disease and Osgood Schlatter disease can coexist. Sinding Larsen Johansson disease is seen in active adolescents typically between 10-14 years of age. Children with cerebral palsy are particularly prone to it.
Both Sinding Larsen Johansson disease and Osgood Schlatter disease can coexist. Sinding Larsen Johansson disease is seen in active adolescents typically between 10-14 years of age. Children with cerebral palsy are particularly prone to it.
The disease most often is seen in males who play sports like football, running, volleyball, gymnastics. Norwegian physician Christian Magnus Falsen Sinding-Larsen in 1921 and Swedish physician Sven Christian Johansson in 1922 had described the same entity independently.
Pathophysiology
The Sinding-Larsen-Johansson syndrome is caused by persistent traction at the cartilaginous junction of the patella causes chronic stress injury with overuse of the patella-patellar tendon junction. Strain due to repetitive traction by the patellar tendon on the lower pole of the patella [which is still partly cartilaginous in adolescents] during quadriceps muscle contraction leads to cartilage damage, swelling and later to tendon thickening and fragmentation of the lower pole of the patella and sometimes to bursitis.
Presentation
Clinically it is characterized by activity-related pain localized to the anterior aspect of the lower pole of the patella. On examination, there is inferior patella tenderness and focal swelling may be noted.
Imaging
Xrays may be normal or may show thickening of the proximal patellar tendon may be seen with stranding of the adjacent portions of Hoffa’s fat pad [Fat that is situated under and behind the patella bone within the knee.] Dystrophic calcification or ossification may be noticed.
Ultrasound shows thickening and heterogeneity of the proximal patellar tendon. Ultrasound can evidence all manifestations of the Sinding-Larsen-Johansson disease.
MRI shows thickening of proximal and posterior part of the patellar tendon.
Differential diagnosis
- Patella avulsion fractures
- Patella stress fracture
- Bipartite patella
- Osgood Schlatter disease – inferior attachment of the patellar tendon into the tibial tuberosity
- Jumper’s knee – same location and similar pathology, but seen in adults.
- Infrapatellar bursitis
Treatment
Rest and restriction of activity for at least 1–2 months that loads knee such as football games and running. NSAIDs and ice may be used in acute episodes or after the activity.
Physiotherapy including quadriceps strengthening exercises are begun. Full recovery usually takes 12–24 months. Stretching and strengthening exercises are started.
Sinding Larsen Johansson disease is self-limiting disease and the pain would disappear when the patella is completely ossified. As the skeleton matures, symptoms usually improve and, in this way, it is regarded as a self-limiting process. However, symptoms may be present for at least a year.