Last Updated on August 2, 2019
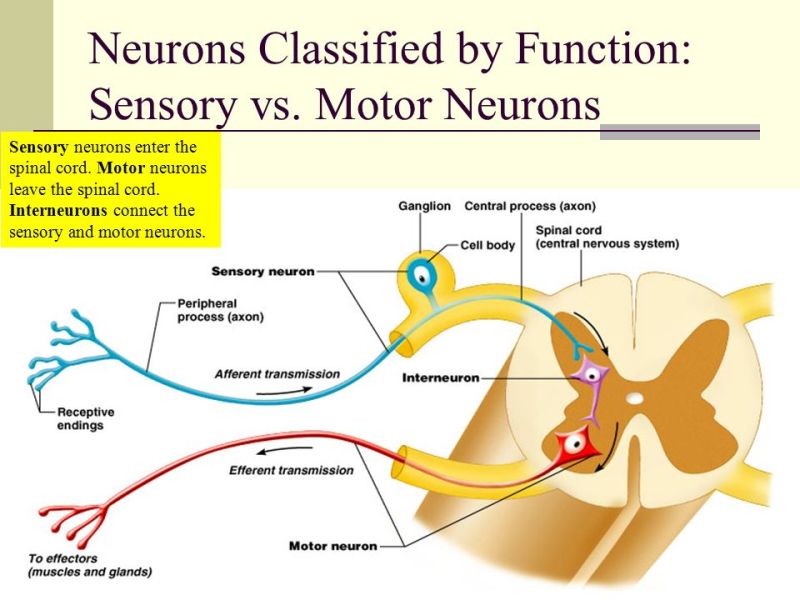
A neuron is a nerve cell. A motor neuron is nerve cell that controls movements of the muscle.

Depending on their location and function, neurons are classified as upper motor neuron or lower motor neuron is a neuron. [More on this in anatomy]
Broadly speaking, upper motor neurons originate in brain and lower motor neurons in spinal cord [Except those of cranial nerves which are from brain directly but are lower motor neurons]
Upper motor neurons transmit the nerve impulses from upper to lower motor neurons and control the behavior of muscles by signaling lower motor neurons.
Lower motor neurons actually signal the muscle to contract.
Both of these neurons when injured, present with their own set of clinical signs.
By looking at those signs, one can conclude the site of injury and reach at the diagnosis.
Suppose a person presents with weakness of upper limb.
If the lesion is in upper motor neurons [as in stroke], the cluster of signs would be different from if the weakness is due to injury to peripheral neurons such as in brachial plexus injury.
Relevant Anatomy
The brain and spinal cord constitute central nervous system.
The central nervous system is divided in white and gray matter. The white matter consists of axons [An axon is a long, slender projection of a nerve cell, or neuron ] and oligodendrocytes [a glial cell concerned with the production of myelin in the central nervous system] while the gray matter consists of neurons and unmyelinated fibers.
The gray matter contains neuron-bodies in brain whereas white matter that form tracts and commissures.
The spinal cord, by spinal nerves which connect the spinal cord to skin, joints and muscles.
This allows for efferent motor as well as afferent sensory signals and stimuli.
Efferent [which take away towards periphery] neural pathways control voluntary and involuntary motions of muscles and afferent [which take signals towards CNS] pathways are sensory in nature.
Sensory input fibers are afferent in nature and motor input fibers are efferent.
Cranial nerves are 12 peripheral nerves of the peripheral nervous system that connects to brain directly or through intermediate ganglia.[Two pairs of cranial nerves; the olfactory nerves and the optic nerves are often considered structures of the central nervous system. ]
Grey matter in spinal cord present as three columns: the anterior grey column, the posterior grey column, and the lateral grey column.
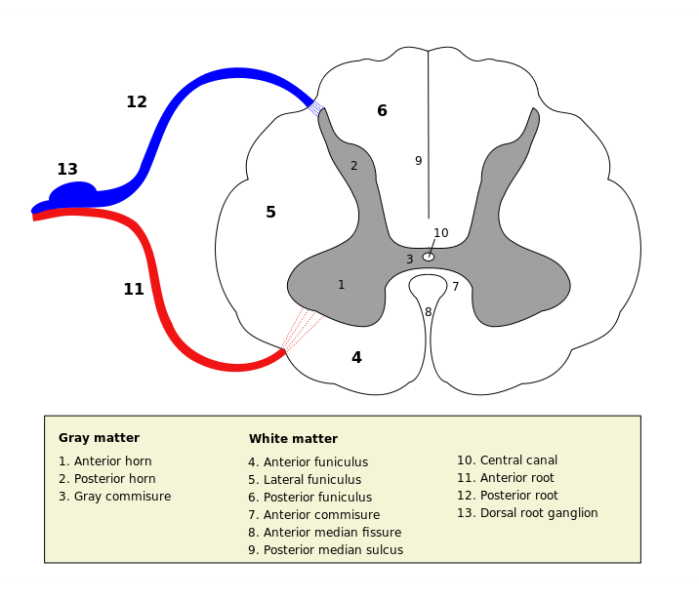
The anterior grey column contains motor neurons that affect the skeletal muscles.
The anterior grey column, also known as the anterior horn of spinal cord, comprises three different types of neurons: large alpha motor neurons, medium gamma motor neurons, and small neurons thought to be interneurons.
Upper Motor Neuron
Upper motor neurons are motor neurons that originate either in the motor region of the cerebral cortex or in the brain stem and carry motor information down to the lower motor neurons.
The primary motor cortex or precentral gyrus, is one of the most important areas in the frontal lobe.
The fibers decussate (intersect) within the lower medulla oblongata of brainstem to form the lateral corticospinal and the fibers that do not decussate pass through the medulla to form anterior corticospinal tracts.
The major function of this pathway is fine voluntary motor control of the limbs and control of body postures.
Some fibers from the motor cortex go to several nuclei in the pons and medulla oblongata and are called corticobulbar tracts. These are involved in control of facial and jaw musculature, swallowing and tongue movements.
The pyramidal tract is name given to both the corticospinal and corticobulbar tracts.
[ The pyramidal tracts are named because when descending from the internal capsule to the brain stem, converge to a point from multiple directions giving the impression of inverted pyramidal bumps on either side of the medulla of the brain.]
The other tracts are colliculospinal tract, rubrospinal tract, vestibulospinal tract and reticulospinal tract are extrapyramidal tracts, and target the neurons in the spinal cord involved in reflexes, locomotion, complex movements, and postural control. ]
The upper motor neuron descends in the spinal cord to the level of the appropriate spinal nerve root.
At this point, the upper motor neuron synapses with the lower motor neuron, each of whose axons innervate a fiber of skeletal muscle.
Lower Motor Neuron
Anterior grey column or anterior horn of the spine harbors the motor neurons. It is also called ventral horn.
At any given level of spinal cord, there would be descending upper motor neurons for the lower segment and lower motor neurons for that segment.
For example, at spinal segment D4 level, there would be
- Descending neural pathways for D5 and lower segments [upper motor neuron]
- Muscle fibers for the muscles supplied by D4 segment [Lower motor neuron]
Cranial nerve nuclei of the brainstem and cranial nerves with motor function are also lower motor neurons.
Thus to sum up following constitute lower motor neurons
- Motor neurons located in either the anterior grey column
- Anterior nerve roots (also called spinal lower motor neurons)
- Cranial nerve lower motor neurons
All voluntary movement relies on spinal lower motor neurons, which innervate skeletal muscle fibers and act as a link between upper motor neurons and muscles. Cranial nerve lower motor neurons control movements of the eyes, face and tongue, and contribute to chewing, swallowing and vocalization. Damage to the lower motor neurons can lead to flaccid paralysis.
Lower motor neurons are classified based on the type of muscle fiber they innervate
- Alpha motor neurons innervate extrafusal muscle fibers. [Extrafusal muscle fibers are the skeletal standard muscle that make major mass of muscle.]
- Beta motor neurons and gamma motor neurons which innervate intrafusal muscle fibers [Intrafusal fibers are part of the muscle and serve as specialized sensory organs (proprioceptors) that detect the amount and rate of change in length of a muscle.
Upper Motor Neuron Syndrome
All the lesions of brain lead to upper motor neuron signs. Injury of upper motor neurons is common because of the large amount of cortex occupied by the motor areas, and because motor pathways extend all the way from the cerebral cortex to the lower end of the spinal cord.
The resulting changes in muscle performance that can be wide and varied are described overall as upper motor neuron syndrome
In case of spinal cord insult, the level of injury determines the type of lesions.
Below the level of injury, the signs are of upper motor neuron as the upper motor neuron pathways to lower segments are broken.
At the level of injury, the signs would be that of lower motor neuron.
Causes of Upper Motor Neuron Lesions
- Stroke
- Multiple sclerosis
- Spinal cord lesions
- Acquired brain injury
- Other brain lesions
Presentation of Upper Motor Neuron Lesions
This clinical picture entails a characteristic set of motor deficits.
In acute injury, the muscles supplied becomes flaccid especially in arms and legs. All reflex activity on the affected side is abolished
This initial period of “hypotonia” after upper motor neuron injury is called spinal shock.
It reflects the decreased activity of spinal circuits because of sudden deprivation of input from cortex and brainstem.
After spinal shock is over, the spinal circuits regain much of function for reasons that are not fully understood, eventually leading to following signs
The Babinski sign
When sole of the foot is stroked in a normal adult, the response is is flexion of the big toe, and often the other toes. It is called a flexor response.
After upper motor neuron lesion, the response becomes extensor where the timulus elicits extension of the big toe and a fanning of the other toes. A similar response occurs in human infants before the maturation of the corticospinal pathway and presumably indicates incomplete upper motor neuron control of local motor neuron circuits.
Spasticity
Sapacticity means increased muscle tone, hyperactive stretch reflexes, and clonus. Muscle tone is the resting level of tension in a muscle
It must be noted that in spite of increased muscle tone, the strength is decreased, making muscles actually weaker.
This kind of paralysis is called spastic paralysis.
The level of injury also determines the severity of the spasticity.
Spasticity that follows damage to descending pathways in the spinal cord is less marked than the spasticity that follows damage to the cortex or internal capsule.
Spasticity is probably caused by the removal of inhibitory influences exerted by the cortex and an abnormal increase in the gain of the spinal cord reflex due to loss of descending inhibition
Hyporeflexia of superficial reflexes.
There is a decreased vigor and increased threshold of superficial reflexes like the corneal reflex, superficial abdominal reflex or cremasteric reflex in males. The mechanism is not known and these should not be confused with stretch reflexes which are hyperactive.
Loss of the ability to perform fine movements
The ability to execute fine movements such as independent movements of the fingers is lost. AS upper limb is more concerned with finer movements, the disability is more pronounced in upper limbs.
An upper motor neuron lesion is also known as pyramidal insufficiency.
Pronator Drift
When patient is asked to stand with eyes closed and arms held straight out and hands supinated, the patient is not able to maintain thisposition. Their occurs pronation and downward drift besides other issues like standing problems
Lower Motor Neuron Syndrome
The symptoms that arise from damage to the lower motor neurons of the brainstem and spinal cord are referred to as the lower motor neuron syndrome.
In the spine, a lower motor neuron lesion is a lesion which affects nerve fibers traveling from the ventral horn or anterior grey column of the spinal cord to the relevant muscle(s) – the lower motor neuron.
Causes of Lower Motor Neuron Lesion
- Lesion of peripheral nerves that sever the axons
- Viral infection
- Guillain–Barré syndrome
- Polio
- Cauda equina syndrome
- Amyotrophic lateral sclerosis.
- Peripheral nerve injuries
- Nerve root injuries [as PIVD]
Presentation of Lower Motor Neuron Lesions
Lower motor lesions lead to following signs
Flaccid Paralysis
One major characteristic of a lower motor neuron lesion is flaccid paralysis – paralysis accompanied by loss of muscle tone.
Damage to lower motor neuron cell bodies or their peripheral axons results in paralysis of the affected muscles
In addition there would be a loss of reflexes (areflexia) due to interruption of the efferent (motor) limb of the sensory motor reflex arcs.
Damage to lower motor neurons also entails a loss of muscle tone.
[Compare with upper motor neuron lesion- spastic paralysis and hypertonia]
Muscle Atrophy
This is a late effect where wasting of muscle is seen. The limb appears thinner due to wasting. The wasting is affected by denervation.
Fibrillations and Fasciculations
Fibrillations are spontaneous twitches in the muscle fibers due to change in the excitability of denervated muscle fibers.
Fibrillations are result of abnormal activity of injured ? motor neurons in the case of fasciculations.
These spontaneous contractions can be readily recognized in an electromyogram, which is a helpful clinical tool.
Main Difference Between Upper and Lower Motor Neurons
These are depicted in following table
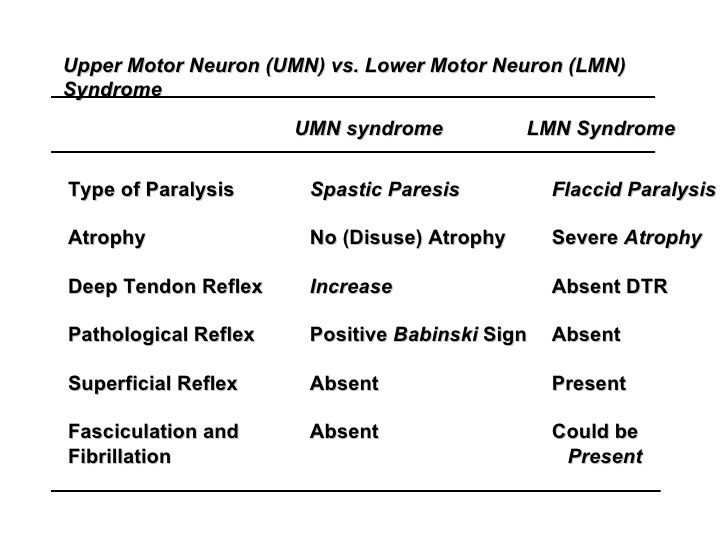
Knowing these differences is of utmost imprtance in the clinical examination.