Last Updated on November 12, 2019
Ankle pain can originate in ankle joint or surrounding tissues. The ankle joint is a weight-bearing hinged joint and ankle pain can be caused by injury or disease of the ankle joint or surrounding tissues.
The present article is a general overview of causes and treatment of ankle pain.
Relevant Anatomy
[Read detailed anatomy of ankle joint]
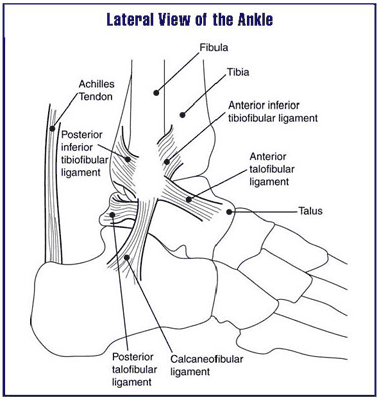
The ankle joint anatomy is formed by the meeting of three bones.
- The end of tibia including the medial projection called medial malleolus.
- The lower end of fibula also called lateral malleolus
- Dome of the talus bone
The stability of the ankle joint is provided by lateral and medial ligaments. The ankle joint is surrounded by a fibrous
Tendons passing through all around the ankle and fibrous structures also contribute to the stability. Notable are
- Achilles tendon behind the ankle attaching at the back of the heel.
- Posterior tibial tendon passing behind the medial malleolus.
- Peroneal tendon passes behind the lateral malleolus to attach into the foot.
Causes of Ankle Pain
Ankle Injuries
Ankle sprains are one of the common musculoskeletal injuries. Sprains are partial or complete ligament tears. Both medial and lateral ligament can get injured.
The typical injury is caused by twisting of the ankle. There might be a popping sensation.
Fractures around the ankle occur as a result of greater force. This could be due to twisting of the ankle, falls or motor vehicle injuries.
Depending on the type of force the ankle can get dislocated too.
Ankle injuries result in immense pain and are associated with swelling. Movements of the ankle are painful.
Tenderness would be present over the injured part.
With a severe ankle injury, such as from a motor vehicle accident, dislocation of the ankle joint can occur. Ankle dislocation is a serious injury and generally requires a surgical repair. A dislocated ankle occurs when there is complete damage and disruption of the ligaments that support the ankle joint.
Tendinitis
Tendinitis or tendonitis) is inflammation of the tendon. Common tendons around the ankle to be involved by tendinopathy [a better term which includes both tendinosis and tendinitis] are the Achilles tendon, the posterior tibial tendon, or the peroneal tendon.
Tendinitis can result from trauma or underlying inflammatory diseases or illnesses such as rheumatoid arthritis, ankylosing spondylitis, and other seronegative spondyloarthropathies.
All forms of tendinitis cause pain, swelling, and tenderness in the tendon area involved. Depending upon the causation, the development may be rapid or slow.
Tendinosis can lead to tendon rupture. Achilles tendon rupture is quite common in middle-aged recreational athletes. It occurs without much trauma and often spontaneously. There is a popping sound and the patient walks awkwardly as there is a loss of strength of plantar flexion.
The treatment is often Surgical.

Bursitis
Two main bursae that can cause ankle pain are
- Retrocalcaneal or subtendinous bursa [which is located between the Achilles tendon and the calcaneus]. This bursa is anterior to Achilles tendon.
- Subcutaneous calcaneal bursa, superficial to the Achilles tendon. Also called the Achilles bursa. This bursa is located between the skin and posterior aspect of the distal Achilles tendon.
Inflammation of either or both of these bursae can cause pain at the posterior heel and ankle region. Retrocalcaneal bursitis is fairly common.
Arthritis
Primary osteoarthritis of the ankle is less common in the ankle than knee or hip. The presence of degenerative changes in ankle joint may occur in the knee or hip malalignment or muscular imbalances.
Valgus or varus ankles can give rise to secondary osteoarthritic changes. But ankle joint can be involved in rheumatoid arthritis, psoriatic arthritis, reactive arthritis or pseudogout.
Malunion of ankle fractures may also lead to degenerative changes.
Osteochondritis Dissecans
Osteochondritis dissecans is a condition in which a segment of articular cartilage with its underlying subchondral bone gradually separates from the surrounding osteocartilaginous tissue.
The separation of the fragment may be partial or complete.
Osteochondritis dissecans affects two forms. Juvenile which affects children between age 5-15 years and adult form that affects adolescents with closed physes and adults.
In the ankle, it affects the posteromedial aspect of the talus 56% of the time and in the anterolateral aspect 44%.
Osteochondritis dissecans has a male-to-female ratio of 2-3 to 1.
The exact cause is not known.
Osteochondrosis
Sever Disease refers to osteochondrosis of apophysis of the calcaneum.
Sever disease or calcaneal apophysisits was first described by JW Sever in 1912. Sever disease is a painful inflammation of the calcaneal apophysis. It is considered as an adolescent nonarticular osteochondroses.
The repetitive pull of the tendocalcaneus on its insertion is thought to be responsible for this entity. The problem occurs in growing age and occurrence is more in children who actively participate in sports.
The typical pain is behind the ankle.
Plantar fasciitis
Plantar fasciitis is a common cause of heel pain and occurs due to degenerative changes at the insertion of the plantar fascia on calcaneal tuberosity. The plantar fascia is the most common cause of heel pain for which professional help is sought.
Pain on weight-bearing is a typical complaint.
A heel spur is commonly found in plantar fasciitis patients, but many asymptomatic persons also have heel spurs.
Plantar fasciitis could be bilateral in almost one-third of cases. It is usually seen in people aged 40-60 years. Early incidence is noted in people with spondyloarthropathies.
Infectious Arthritis
The infection of the ankle joint can be caused by many organisms and is common in children than adults.
A typical bacterial arthritis presents with immense pain, immobility, and welling of the joint. The joint is swollen and red. High-grade fever is often associated.
Tuberculosis of the ankle joint is less common and does rarely has an acute presentation. the typical presentation is the pain on weight-bearing and swelling of the joint.
Posterior Tibial Tendon Dysfunction
Posterior Tibial Tendon Dysfunction is often called adult-acquired flatfoot. Usually, it occurs in one foot but some people may develop it in both feet. Untreated, It is usually progressive.
It is generally caused by overuse of the posterior tibial tendon by activities that involve the tendon, such as running, walking, hiking or climbing stairs.
Pain, swelling, a flattening of the arch and an inward rolling of the ankle are usual symptoms.
The pain is the inside of the foot and ankle along the course of the tendon.
Later, as the arch begins to flatten, there may still be a pain on the inside of the foot and ankle.
The foot and toes begin to turn outward and the ankle rolls inward.
Lab Studies in Ankle Pain
CBC, ESR, CRP, Rheumatoid factor, antinuclear antibodies, and HLA B-27etc would help to differentiate between inflammatory and infectious causes. Aspiration and culture of the organism from the joint fluid would further help to confirm the infectious causes. PCR for tuberculosis may suggest the presence of mycobacteria.
Imaging
X-rays are the basic imaging required. Anteroposterior and lateral views are done. X-rays are able to show bony injury, joint subluxation or dislocation. They can also show advanced infection of the bone.
Reduction of joint space would be seen in chronic arthritis.
In soft tissue injuries, the x-rays would be normal.
In complex periarticular injuries like pilon fractures, CT with 3D reconstruction would help.
MRI is able to reveal soft tissue injuries better and grade them. Joint pathologies, talar lesions, and tendon ruptures would be better revealed by MRI. It is also able to differentiate between inflammatory and infectious pathologies.
Treatment
The actual specific treatment would depend on the cause of ankle pain.
Mild ankle injuries are initially treated with ice, rest, and limiting the amount of walking and weight-bearing on the injured ankle. The leg can be elevated to reduce swelling, and crutches are often recommended to avoid further trauma to the injured ligaments.
Anti-inflammatory medications can be given to reduce local inflammation. Ice packs help decrease further swelling of the area and can reduce pain.
Patients with severe injuries are placed in immobilization casts or may require surgical repair.
[More on the treatment of sprains ]
[More on the treatment of ankle fractures.]
Immediate treatment of tendinitis involves immobilizing the area, elevation, and limiting weight-bearing, applying ice, and using nonsteroidal anti-inflammatory drugs (NSAIDs) to decrease inflammation.
Achilles tendon ruptures require orthopedic surgical repair.
[More on the treatment of Achilles tendinosis ]
[More on the treatment of Achilles rupture]
A patient with bursitis is also treated by rest and anti-inflammatory drugs.
[Read more about the treatment of bursitis]
Plantar fasciitis may require modification of shoe wear, heel cushion, and anti-inflammatory drugs.
[More on the treatment of plantar fasciitis]
Arthritis requires rest and NSAIDs. Weight relieving assistance like stick or walker may be prescribed.
Specific treatment may be initiated for rheumatoid arthritis and other inflammatory arthritides.
[More on the treatment of rheumatoid arthritis]
Bacterial arthritis is treated by the use of antibiotics and drainage of pus if required. Antitubercular treatment is given for tubercular arthritis of the ankle. For resting the joint, a splint may be applied.
Osteochondrosis is treated by the rest of the ankle joint, avoidance of activity and NSAIDs.
Osteochondritis dissecans may be treated with rest and medication or need arthroscopic removal.