Last Updated on March 7, 2020
Adhesive capsulitis is disease of shoulder that leads to pain and contracture of shoulder. It is commonly referred to as frozen shoulder.
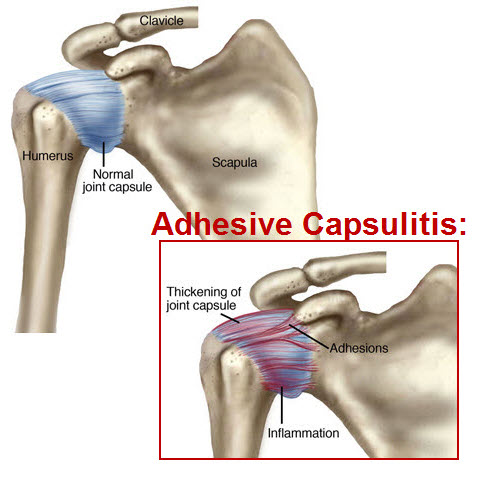
Adhesive capsulitis is a poorly understood condition that is characterized by physical findings like thickening of the synovial capsule and adhesion to surrounding tissues.
It is found in 3-5% of the population and is most common in females >5o years.
It is found in 20% people who have diabetes. Though it is said to be self-limiting disease that resolves within 1–3 years, some studies have suggested that 20- 50% of patients with adhesive caspulitis suffer long-term range of motion deficits for longer period.
Though it rarely occurs simultaneously bilaterally, sequential bilateral occurrence has been reported. Bilateral occurrence is more common in diabetics.
Adhesive capsulitis is associated with conditions like diabetes [most common], hyperthyroidism, hypothyroidism, hypoadrenalism, Parkinson’s disease, cardiac disease, pulmonary disease, stroke, after cardiac surgery, cardiac catheterization, neurosurgery, and radical neck dissection.
Classification of Adhesive Capsulitis
Adhesive capsulitis is classified into two categories
Primary Adhesive Capsulitis
- Insidious and idiopathic.
- Gradual progression of symptoms
Secondary Adhesive Capsulitis
- Due to trauma or subsequent immobilization
- Symptom progression is rapid
Pathophysiology of Adhesive Capsulits
The pathophysiology of frozen shoulder is not clear.
Pain starts first and causes limitation of motion. Prolonged immobilization causes many changes like
- Decreased collagen length
- Fibrofatty infiltration into the capsular recess
- Ligament atrophy resulting in decreased stress absorption
- Collagen band bridging across recesses
- Random collagen production
- Altered sarcomere number in muscle tissue
Glenohumeral joint synovial capsule is often involved in this disease process. But structures outside the synovial capsule such as the coracohumeral ligament, soft tissues in the rotator interval, the subscapularis muscle, and the subacromial bursae are also involved
Neurologic factors seem to be the principle mediators of the pain, whereas a process resembling fibromatosis causes the contracture.
The research also suggests the presence of autonomic sympathetic dysfunction not dissimilar to complex regional pain syndrome. In fact there are many parallels between the diseases and both have common risk factors like diabetes, thyroid disease, and dyslipidemia.
CNS neural sensitization is also thought to play a part.
Destruction of terminal sensory nerve fibers as a result of myxoid globular degeneration, a normal aging phenomenon may play a role in the apparent dysfunction of the nervous system.
Ischemia is thought to be the dot connector element of Ischemia of separate pathophysiologic entities. Pre-existing microvascular disease, often related to hypertriglyceridemia or diabetes, may predispose them to ischemia of the connective tissues of the glenohumeral joint capsule causing local release of free radicals and a platelet-derived growth factor that can initiate a cycle of fibroblastic hyperplasia and excessive deposition of collagen and glycosaminoglycans.
Phases of Adhesive Capsulitis
Adhesive capsulitis presentation is generally broken into three distinct stages
Freezing or Painful Stage
Pain is major feature and patient often do not seek consultation
The patients may not present during this stage because they think that eventually the pain will resolve. As the symptoms progress, pain worsens and shoulder becomes stiff. Usually, this is the stage where patient seeks a medical consultation.
This phase typically lasts between 3 and 9 months and is characterized by an acute synovitis of the glenohumeral join
Frozen Stage or Transitional Stage
Most patients will progress to the this stage. The pain may worsen or stay the same but use of the arm becomes limited. External shoulder rotation is most commonly limited, followed closely by shoulder flexion, and internal rotation.
This phase lasts for 4-12 months.
Thawing or Regressing Stage
Range of motion begins to improve.This stage lasts anywhere from 12 to 42 months and is defined by a gradual return of shoulder mobility.
Presentation of Adhesive Capsulitis [Symptoms and Signs]
The typical presentation is insidious onset pain which progresses over a period. The pain is usually present [or worse] at night or activities involving shoulder. The movements tend to stretch the capsule. For example
- Combing one’s hair or reaching for seatbelt – abduction and Internal rotation
- Reaching for one’s back pocket – Extension and internal rotation of the shoulder.
Progression of the pain leads to pain even at rest and pain that gets aggravated by slight movement of the shoulder, stress, exposure to cold or vibration, and weather changes.
During the thawing phase, the pain usually is less intense than it is in the other phases.
On examination, in early phase, the shoulder may not have any sign except for terminal restriction of motion especially in the activities that stretch the capsule such as combined abduction and external rotation (combing one’s hair) or combined extension and internal rotation (such as reaching to scratch one’s midback).
In later stage, the contracture of the glenohumeral joint becomes apparent. This stage may occur only several months after the onset of symptoms.
Progressive limitation of the passive range of motion occurs. First motion to be affected is external rotation, then abduction internal rotation, and flexion. Extension and horizontal adduction tend to be least affected.
Compensatory inverted scapulothoracic motion may be noticed in some cases.
Clinical examination must exclude concomitant systemic rheumatologic, inflammatory, metastatic, or infectious disorders.
The diagnosis of Adhesive capsulitis syndrome is clinically based on the history and physical findings.
Differential Diagnoses
- Biceps Rupture
- Biceps Tendinopathy
- Cervical Myofascial Pain
- Cervical Spondylosis
- Cervical Sprain
- Brachial Plexopathy
- Rheumatoid Arthritis
- Rotator Cuff Disease
- Shoulder Pain in Hemiplegia
- Thoracic Outlet Syndrome
Lab Studies
There is no investigation for adhesive capsulitis. But investigations are done to rule out associated diseases like diabetes, hyperthyroidism, and hypertriglyceridemia in patients with FS.
Imaging Studies
Basic x-ray views of the shoulder are done to determine shoulder contour, joint status and any abnormality if present.
Gallium nuclear scanning may be indicated in immunocompromised patients suspected of septic arthritis.
Other sophisticated imaging like computed tomography, CT arthrography, ultrasonography and MRI are rarely needed.
Treatment of Adhesive Capsulitis
Drugs for Pain and Inflammation Control
NSAIDs and corticosteroids are the drugs that work to reduce inflammation and relieve symptoms though they may not alter the natural history of adhesive capsulitis.
NSAIDs are a reasonable first choice for treatment.
Steroids may reduce pain early on better than rehabilitation or placebo but their benefits are not maintained long term. They may be considered when short-term gain is necessary for a particular event.
Local Injections
Corticosteroid Injections
There is evidence of short term benefit of glenohumeral [intra-articular] or subacromial [intrabursal] corticosteroid injections and should be considered. In the long term, they are not superior to placebo but they are superior to supervised physical therapy.
However, blind procedures may result in inaccurate placement in up to 60% cases. Injections performed under radiological imaging like ultrasound have better accuracy.
An intrabursal injection of corticosteroid can be used as a complementary treatment to intra-articular injection
Sodium Hyaluronate Injections
Sodium hyaluronate has a metabolic effect on the articular cartilage and , synovial tissues, and liquid. Though concrete evidence is not yet established, intra-articular injections of sodium hyaluronate may be an alternative treatment especially in those patients where corticosteroid injections are contraindicated.
Nerve blocks
Suprascapular nerve block
The suprascapular nerve block has been found to improve pain and range of motion earlier than corticosteroid injections. Pain decreased and range of increased more rapidly and more completely with the nerve block.
Capsular Distension Injections
Under under local anesthesia, the joint is injected to its limits with local anesthetic to attempt to stretch the capsule. Intraarticular injection is given after the capsule has been stretched to maximum.
One study recommends distension arthrography in the second stage of disease that is not progressing, despite the patient’s participation in physical therapy. [1]
Surgical treatment
Surgical treatment should be considered only in cases of failed non-operative treatment.
Manipulation under anesthesia
Manipulation under anesthesia as a means of treatment has been advocated. This method allows return of ROM in the operating room. Immediate postoperative physical therapy can be initiated with this form of treatment. Recent studies show manipulation alone to be ineffective [2]
Arthroscopic release and repair
Arthroscopy is an excellent additional tool for addressing the shoulder with adhesive capsulitis. The contracted structures are released to allow ROM to return with manipulation if necessary.
Physical Therapy and Exercises
Physical therapy alone does not improves function in the treatment of adhesive capsulitis. Physical therapy associated with an intra-articular injection of corticosteroid improves function and ROM more rapidly than does injection alone.
Prognosis of Adhesive Capsulitis
The prognosis for patients with FS is generally favorable.
Early mobilization of the shoulder is crucial in the early stages of FS syndrome.
Complications of FS include constant pain, loss of functional use of the upper extremity, recurrence, and permanent disability of the shoulder.
Improvements in pain and disability after the treatment of adhesive capsultis usually occur over months and not over days or weeks.
Workers whose tasks require them to move their shoulder may have long-term difficulties in resuming their previous job.
References
- Vad VB, Sakalkale D, Warren RF. The role of capsular distention in adhesive capsulitis. Arch Phys Med Rehabil. 2003 Sep. 84(9):1290-2.
- Hazleman BL. The painful stiff shoulder. Rheumatol Phys Med. 1972 Nov. 11(8):413-21.
-
Curr Rev Musculoskelet Med. 2008 Dec; 1(3-4): 180–189.Published online 2008 May 23.
doi: 10.1007/s12178-008-9031-6