Last Updated on October 29, 2023
Proximal femur fractures are fractures that occur in the femur in the hip region. These fractures are further divided into different subsets depending on the specific site involved. Proximal femur fractures tend to occur in two populations – in older patients where these result from low energy trauma in osteoporotic bones and in younger patients following high energy trauma like motor vehicle accidents.
Classification of Proximal Femur Fractures
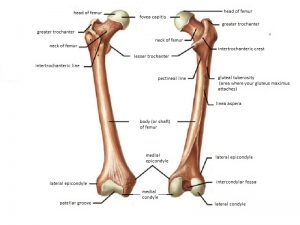
Traditionally, proximal femur fractures are therefore divided into groups based on their location with regard to the capsule, i.e. whether they are intracapsular or extracapsular.
Intracapsular fractures
These fractures include the sites within the lining of the hip joint capsule. These are associated with injury to the blood supply to head of the femur. A compromised supply may result in avascular necrosis of femoral head.
These include
- Femoral head fractures- They usually occur secondary to femoral head dislocation.
- Femoral neck fractures – Depending on fracture location these are further classified as
- Subcapital fracture – just below the head of the femur
- Transcervical fracture – through mid neck
- Basicervical fracture – through base of the neck
Extracapsular fractures
These fractures are present outside the capsule and do not cause the same degree of vascular damage as intracapsular fractures and therefore can be treated differently. The trochanteric fractures are extracapsular injuries.
 Clinical Presentation of Proximal Femur Fractures
Clinical Presentation of Proximal Femur Fractures
The clinical presentation of the proximal femur fractures can vary depending on the type, severity, and cause of the fracture.
Patients with displaced fractures usually cannot stand or ambulate. However, patients with nondisplaced or impacted fractures may be ambulatory and experience minimal pain.
Few patients present with thigh or groin pain without any history of trauma. These patients should be suspected to have with a stress fracture of the proximal femur. They should be enquired about any recent changes in the type, duration, or frequency of physical activity.
In patients in whom no significant history about activity or trauma is available, pathological fracture must be considered.
Most proximal femur fractures in elderly persons are the result of a low –energy fall, whereas in young adults they are more often caused by high energy trauma.
In the latter, a search for associated head, neck, chest, and abdominal injuries.
Patients with displaced proximal femur fractures exhibit the classic presentation of a shortened and externally rotated extremity. There may be tenderness to palpation in the area of the greater trochanter. Ecchymosis may be present and should be noted.
Range-of-motion testing of the hip will be painful and should be avoided. Although the neurovascular injury is rare after hip fracture, careful evaluation is nevertheless mandatory.
Medical History
It is important to obtain a careful medical history, as preexisting medical comorbidities affect both treatment and prognosis. Cardiopulmonary diseases (congestive heart failure, intermittent myocardial ischemia, chronic obstructive pulmonary disease) is a common preexisting medical condition that affects fracture management in the elderly.
These medical disorders affect the patient ability to undergo surgery, and participate in rehabilitation.
Neurological conditions such as parkinsonism, Alzheimer’s disease, and the residual effects of a previous cerebrovascular event must also be considered during treatment. Treatment of these patients may be complicated by the presence of osteopenia, spasticity, and/ or contracture.
For patients with Alzheimer’s disease and severe cognitive dysfunction, a treatment plan that requires a high degree of patient cooperation would not be right.
A medication history is particularly important in elderly patients.
Preinjury Functional Status
For a reasonable management plan, a detailed history of the patient’s preinjury function must be taken because treatment goals for an active, independent ambulatory differ from those for a nonambulatory.
In the case of ambulators, surgical treatment followed by aggressive rehabilitation should be considered. A nonambulatory would be treated by non-operative treatment and early bed-to-wheelchair mobilization.
Ambulatory status is best defined as one of four types.
- Community ambulator who walks indoors and outdoors.
- Household ambulator who walks only indoors
- Nonfunctional ambulator who walks only during physical therapy sessions
- Nonambulator who is wheelchair bound but may be able to transfer from bed to chair.
Imaging
X-rays
The standard radiographic examination of the hip includes
- Anteroposterior view of the pelvis including proximal femora
- Cross-table lateral view of the involved proximal femur.
The AP radiograph allows comparison of the involved side with the contralateral side.
Lateral x-ray can help to assess posterior comminution of the femoral neck and proximal femur.
An internal rotation [10-15 degrees] view of the injured hip may be helpful to identify nondisplaced or impacted fractures. [Internally rotating the involved femur 10 to 15 offsets the anteversion of the femoral neck and provides a true AP view of the proximal femur.]
MRI
MRI is done when a proximal femoral fracture is suspected but not apparent on standard radiographs.
Bone Scan
The indication is same as that of MRI but it may take two or three days after the fracture before a bone scan becomes positive.
Lab Studies
Complete blood count, electrolytes. blood urea nitrogen and creatinine, an electrocardiogram, and a chest radiograph are the usual investigations, . An arterial blood gas analysis is also carried in patients with pulmonary disorder.
Preoperative Medical Evaluation
A medical evaluation helps to determine whether a patient is sufficiently medically stable for operative treatment and to help prevent and treat medical complications in the perioperative period. Older people tend to have more coexisting medical conditions that increase surgical risk. Depending on the patient profile multiple specialists may be needed.
Cardiac Disease
Preoperative stress test should be considered for patients [dipyridamole thallium stress test or a dobutamine echocardiogram stress test] in
- Unstable cardiac profile
- New-onset angina or change in angina pattern has undergone a change. A patient with a fracture of the proximal femur would require a.
- Mechanism of injury suggests a cardiac event
Patients with poorly controlled hypertension ( systolic blood pressure> 200 or a diastolic blood pressure > 105) are at increased risk for cardiac arrhythmias and myocardial ischemia.
Patients who have well-controlled blood pressure or mildly elevated blood pressure[systolic blood pressure greater than 110] prior to surgery behave similarly to patients with normal blood pressure patients. Patients with mildly elevated blood pressure (i.e., those with) also behave similarity to normotensive patients.
Pulmonary Disease
A preoperative pulmonary workup is not warranted if the patient has mildly symptomatic pulmonary disease. Those with more severe symptoms, a chest radiograph, and arterial blood gas level are obtained.
If both are normal, the patient is cleared for surgery.
Treatment of Proximal Femur Fractures
These patients especially the elderly should be rapidly mobilized to avoid the complication of prolonged recumbency like decubitus ulcers, atelectasis, urinary tract infection, and thrombophlebitis.
All patients who sustain a hip fracture should be admitted to the hospital and maintained on bed rest. The leg is kept in the position of comfort—usually slight hip flexion and external rotation, supported by pillows under the knee.
The surgery should be performed as soon possible after stabilization of all comorbid medical conditions.
Perioperative Medical Management
Diabetes
Oral hypoglycemic agents are usually stopped the morning of surgery. Serum glucose levels are checked every 4 to 6 hours, and sliding scale low dose regular insulin is given to prevent severe hyperglycemia.
Intervenous fluids should not contain glucose. Oral hypoglycemic agents are resumed when the patients is eating well.
Anemia
Healthy people can tolerate a hemoglobin level as low as 8.0g/dl. Routine transfusions are not to be given to, rather it should be done only when required as per expected blood loss.
Renal Disease
The elderly are at increased risk of developing renal failure in the perioperative period and elderly persons with increased BUN and creatinine levels are at even higher risk of developing renal failure.
The best method to prevent renal failure is to optimize the patient medically before surgery. Blood pressure and hydration should be well optimized. Nephrotoxic drugs should be avoided.
Corticosteroid Use
Any patient who has been using corticosteroids within the past 2 years requires preoperative stress doses of corticosteroids to prevent an Addisonian crisis. Prednisone 25 mg or hydrocortisone 100 mg the night before surgery and the same dose the morning of surgery as well as n the first preoperative day is usually sufficient.
Thromboprophylaxis
Every patient who sustains a fracture of the proximal femur should receive should receive thromboprophylaxis while awaiting surgery.
Prophylactic Antibiotics
Use of prophylactic antibiotics has resulted in a lower incidence of superficial and deep wound infection after hip fracture surgery. The duration of antibiotic treatment, however, remains controversial 24 hours and for 7 days.
Surgical Procedures
The surgical procedure chosen depends on the age of the patient, activity level, anatomical site, and fracture pattern.
Younger patients are treated with closed or open reduction and internal fixation.
Fracture neck of femur is treated as a surgical emergency in young patients.
Elderly patients with poor bone stock may be considered for hip replacement surgery in cases of fracture femoral neck and intertrochanteric fractures.
Subtrochanteric fractures are treated by open reduction and fixation.
Fracture head of femur is treated by open reduction and internal fixation if the fracture fragment is large enough to fix.
Detailed treatment is discussed in specific articles
Rehabilitation
Early mobilization reduces the risks of deep vein thromboembolism, pulmonary complications, skin breakdown, and a decline in cognitive functions.
Moreover, mobilization inspires confidence and encourages the patients.
Apart from mobilization and ambulation, the training treatment goals improving strength, maintaining balance and maintaining range of joint motion.
Mobilization begins on first postoperative day 1. The range of joint motion, muscle strength, and flexibility exercises are added gradually.
Usually, the patient is assisted out of bed into a chair on the first postoperative day. Bed mobility, using a bed pan etc are taught.
Ambulation training is initiated within the first few days depending on the patient profile. Most patients with internal fixation or prosthetic replacement may be allowed to bear partial weight as tolerated.