Last Updated on November 20, 2019
Reactive arthritis is an autoimmune disease that develops in response to genitourinary or gastrointestinal infection or a preceding Chlamydia respiratory infection.
Reactive arthritis is frequently associated with the HLA B27 histocompatibility antigen but its role in the disease is not fully defined.
Mechanism of development of reactive arthritis is not known but antigens are known to cross-react with self-proteins.
The frequency is estimated to be 3.5-5 cases per 100,000.
Reactive arthritis is most common in young men, with the peak onset in the third decade of life. It rarely occurs in children.
Reactive arthritis after gastroenteric infections is equal in both males and females. The disease associated with genitourinary infection is found more in males.
Infections Leading to Reactive Arthritis
Organisms that have been associated with reactive arthritis include the following
- C trachomatis
- Ureaplasma urealyticum
- Neisseria gonorrhoeae
- Shigella flexneri
- Salmonella enterica
- Mycoplasma pneumoniae
- Mycobacterium tuberculosis
- Cyclospora
- Yersinia enterocolitica and pseudotuberculosis
- Campylobacter jejuni and coli
- Clostridium difficile
- Beta-hemolytic and viridans streptococci
Campylobacter is the most common enteric pathogen.
Clinical Presentation
Symptoms of reactive arthritis occur after 14-28 days of gastrointestinal or genitourinary infection. Preceding symptomatic infection does not occur in about 10% of patients.
The patient complains of acute onset fever, fatigue, and malaise. There is asymmetric joint involvement mainly of lower limbs but joints of upper limbs can be affected. Low back pain may occur in about 50% of patients. Migratory or symmetric involvement is also known.
Shoulders, wrists, and elbows may be affected. Small joints of the hands and feet may be involved in severe cases. Dactylitis may also occur. Sacrolilits has been reported especially in HLA B27 patients.
Enthesitis of Achilles insertion or of plantar aponeurosis insertions may cause heel pain. Enthesitis can also occur at ischial tuberosities, iliac crests, tibial tuberosities, and ribs.
Meatal redness and swelling, meatal discharge, vulvovaginitis, circinate balanitis [shallow painless ulcers of the meatus or glans penis] cervicitis, cystitis, and salpingo-oophoritis are also associated.
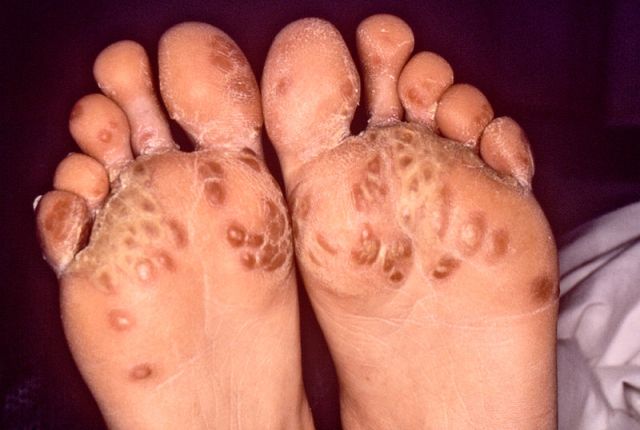
Keratoderma blennorrhagicum [hyperkeratotic skin in the soles, palms, scrotum, trunk, or scalp], erythematous dermatitis, mucal erosions in the mouth, and tongue nail dystrophy can occur as skin lesions.
Conjunctivitis, anterior uveitis (including iritis, iridocyclitis, or cyclitis), scleritis, episcleritis, keratitis, glaucoma, corneal ulceration are commonly associated lesions of the eye.
Abdominal pain, diarrhea may occur.
Aortitis with or without aortic regurgitation and conduction defects of the heart are known to occur.
Noninfectious urethritis, arthritis, and conjunctivitis—is found in only one-third of patients with reactive arthritis.
A large percentage of Reactive arthritis cases present with conjunctivitis or urethritis.
Diagnosis
Asymmetric oligoarthritis [arthritis that involves less than 6 joints], predominantly of the lower extremity along with any of the following would establish the diagnosis of reactive arthritis.
- Conjunctivitis or iritis
- Genital ulceration or urethritis
- Dactylitis toe or heel pain, or other enthesitis
- Cervicitis or acute diarrhea within 1 month of the onset of arthritis
Lab Studies
Inflammatory markers like ESR and CRP are very high. In the acute phase, leucocytosis and thrombocytosis can be present.
HLA-B27 is positive in 65-96% of cases though it is not required for the diagnosis. Rheumatoid factor and antinuclear antibodies are absent.
Joint aspiration may be required to rule out other types of arthritides. The synovial fluid analysis in patients with reactive arthritis shows a high white blood cell count.
Culture of urine, stools, throat and urogenital tract samples are done in order to identify the causative organism.
Serology for detection of Chlamydia must be done. Other tests for chlamydia are direct fluorescent antibody testing, enzyme immunoassay, culture, or nucleic acid probe and polymerase chain reaction (PCR) assay.
Gonorrhea and other types of infectious urethritis must be ruled out by a culture of urethral exudate.
HIV testing must be done in newly diagnosed patients of reactive arthritis.
Antistreptolysin O or anti-DNase B testing in poststreptococcal infection can be done.
Differential Diagnoses
Following conditions have their presentations similar to reactive arthritis and should be considered as differentials
- Ankylosing spondylitis
- Undifferentiated spondyloarthropathy
- Gonococcal arthritis
- Gout
- Inflammatory bowel disease
- Psoriatic arthritis
- Rheumatic fever
- Rheumatoid arthritis
- Septic arthritis
- Seronegative spondyloarthropathies
Imaging
Radiography
Radiological signs are present in only 40-70% of cases, and X-rays may be completely normal in the early part of the disease.
Periosteal reaction and proliferation at sites of tendon insertion, plantar spurs, marginal erosions with adjacent bone proliferation in hand or feet may be noted.
Sacroiliitis and syndesmophytes may be noted in the spine.
Whole-body scintigraphy is a sensitive diagnostic tool for use in screening for enthesopathy and arthropathy.
Positron emission tomography can recognize enthesitis in earlier but is expensive and not readily available.
MRI is more sensitive in detecting sacroiliitis and may be done in children without sacroiliac symptoms.
Ultrasonography may reveal enthesitis more accurately that physical examination would.
Carditis and valvular dysfunction may be found on echocardiography.
Electrocardiography should be performed in patients with a prolonged course of ReA to evaluate for conduction disturbances.
Treatment
Almost 60% of patients have a self-limited course only symptomatic and supportive care is needed.
NSAIDs, physical therapy, and intralesional corticosteroids are the mainstay of therapy. Phenylbutazone may be effective when other NSAIDs fail. Short term low dose steroids like prednisone can be tried.
Antibiotics to treat an underlying infection may be administered.
DMARDs such as sulfasalazine and methotrexate may be used in patients who do not improve with NSAIDs after one month of therapy or where NSAIDs are contraindicated.
Antibiotic treatment is indicated for cervicitis or urethritis but generally not for post-dysenteric ReA
Mydriatics and cycloplegics (eg, atropine) with topical corticosteroids may be administered in patients with acute anterior uveitis.
Local care is done for mucosal lesions.
Systemic corticosteroids may be particularly useful in patients who do not respond well to NSAIDs or who experience adverse effects related to the use of NSAIDs.
Antibiotic treatment does not change the course of the disease, even when a microorganism is isolated.
Sulfasalazine, Methotrexate, etanercept and infliximab, Tocilizumab have been used but further studies are required.
Prognosis
Reactive arthritis usually follows a self-limited course. The symptoms may resolve within 3 months or may take up to one year.
Gastrointestinal infections have a better prognosis than genitourinary infections.
HLA-B27 may predict a worse prognosis and higher recurrence rate.
15-30% of patients with reactive arthritis develop chronic arthritis or enthesitis or spondylitis. Recurrent arthritis can occur in 15-50% patients.
Other reported complications are urethral stricture, aortic root necrosis, glaucoma, cataracts, cystoid macular edema, posterior and anterior synechiae in the eye, opacification of vitreous, ankylosing spondylitis, psoriatic arthritis, and sacroiliitis.