Last Updated on April 27, 2022
Radial head fractures are the fracture of the uppermost disc-shaped part of the radius bone which articulates with ulna at its proximal end through the lesser sigmoid notch and with the humerus. This joint is responsible for forearm pronation and supination.
The radial head fractures may be isolated just to the radial head or they may be part of a complex fracture-dislocation pattern [such as Monteggia fracture dislocation] involving the elbow, distal humerus, or forearm and wrist.
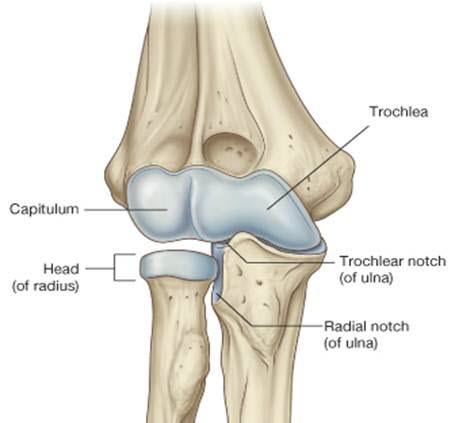
Relevant Anatomy
The elbow joint consists of 3 bones and 3 joints. The bones are the distal humerus, proximal ulna, and proximal radius. The ulnotrochlear joint is between the olecranon process of the ulna and the medial condyle of the humerus. This joint allows only flexion/extension.
The radiocapitellar joint is between the radial head and the lateral condyle of the humerus. This joint is involved in both flexion and extension and forearm rotation. The radioulnar joint is between the radial head and the proximal ulna. This joint allows forearm rotation.
The radial head is entirely intraarticular and thus fracture reduction demands anatomical reduction to reduce the risk of secondary arthritis. There is limited soft tissue around the radial head owing to its intraarticular nature and the fractured fragments need to be carefully assembled to avoid any risk of loose bodies.
The radial head also acts to prevent proximal migration of the radius and if the support is lost, proximal migration of the radius can occur.
The radial head is the most proximal structure of the radius bone and lies about 15 degrees offset from the neck. That means the centers of both are not in a straight line.
It bears an oval-shaped cavity on the superior aspect to articulate with the capitellum. This joint called the radiocapitellar joint is a pivot joint and responsible for more than 50% of load transfer across the elbow.
The ulnar part of the radial head articulates with the ulna at a lesser sigmoid notch to form a proximal radial ulnar joint that is important in forearm supination and pronation.
The anterolateral third part of the radius lacks subchondral bone and gets easily fractured in this region.
Lateral collateral ligament complex stabilizes the elbow on the lateral side. This consists of
- Lateral ulnar collateral ligament
- From posterolateral lateral epicondyle to the proximal part of the supinator crest
- Primary stabilizer in varus and external rotation forces especially in elbow extension
- Radial collateral ligament
- Originates just anterior to the lateral ulnar collateral ligament
- Inserts into the annular ligament
- Annular ligament
- originates and inserts on the anterior and posterior aspect of the lesser sigmoid notch, respectively thus encircling the radial head
- Stabilizes proximal radioulnar joint by maintaining the radial head in contact with ulna
- Accessory lateral collateral ligament
The medial collateral ligament complex stabilizes the medial side of the elbow
It has three bundles
- Anterior bundle is the primary stabilizer of valgus stress
- Posterior bundle
- Transverse bundle
[Read more on Elbow Anatomy]
The normal movements of elbow are flexion/extension [normal – 0-150 degrees] and pronation/supination [85 degrees and 75 degrees respectively.
Mechanism of Injury to Radial Head
The vast majority of fractures of the radial head are sustained due to a fall onto the outstretched hand. The force is transmitted through the radius to the elbow and the head of the radius is driven against the capitellum.
The capitellum thus may also be injured.
Sometimes, a valgus force to the elbow may cause a radial head fracture and fracture of the olecranon. If the medial collateral ligament is torn along with a fracture of the head of the radius, it results in instability of the elbow.
Classification of Radial Head Fractures
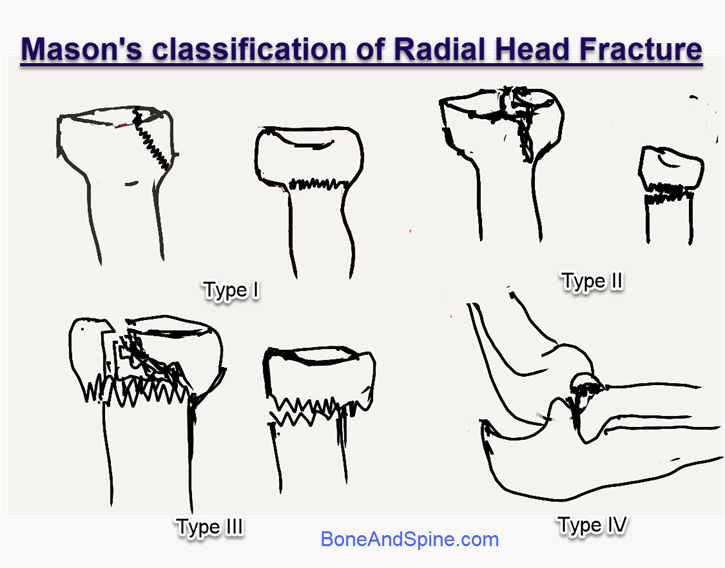
Radial head fracture classification is described by Mason
- Type I
- Simple split-wedge fragment
- Less than 2 mm displacement
- Does not affect forearm rotation
- Type II
- More than 2 mm displacement
- May block forearm rotation
- Type III
- A severely comminuted fracture.
- IIIa – Fracture of the entire radial neck, with the head completely displaced from the shaft
- IIIb- Articular fracture involving the entire head, consisting of more than two large fragments
- IIIc- Fracture with a tilted and impacted articular segment
- A severely comminuted fracture.
- Type IV
- Fracture of the radial head with dislocation of the elbow joint.
Presentation of Radial Head Fractures
There would be a history of fall on an outstretched hand or blunt trauma. There is swelling on the lateral aspect of the elbow in case of isolated radial head injury.
Tenderness and decreased motion would be present.
The wrist should be examined for the stability of the distal radioulnar joint. Elbow stability needs to be assessed.
The range of motion of the elbow joint should be assessed for both flexion-extension and pronation/supination. Any block to the movement needs to be identified.
Associated injuries should be looked for.
Following injuries are associated with radial head fractures and should be looked for
- Fractures of the capitellum
- Fractures of the distal radius
- Dislocation of the distal radioulnar joint (Essex Lopresti Fracture)
- Rupture of medial collateral ligament
- Rupture of the triceps tendon
- Dislocation of elbow
A combination of radial head fracture, medial collateral ligament injury, and coronoid process fracture is known as the terrible triad of the elbow.
Tests for Stability
- Elbow
- Lateral pivot shift test- for lateral stability
- Valgus stress test – for medial collateral ligament
- Distal Radioulnar Joint
- Wrist tenderness
- More than 50% translation in the sagittal plane as compared to the opposite side
- Interosseous membrane
- Tenderness along interosseous membrane
- Radius pull test
>3mm translation
Imaging
X-rays
X-rays in the anteroposterior, lateral, and oblique planes of the elbow are usually sufficient to diagnose the fracture.
Mostly, the radial head fractures can be assessed adequately with anteroposterior and lateral views of the elbow. The radial head must be aligned with the capitellum on all views.
In occult or minimally displaced fractures that are not surely visible on x-ray, may see anterior/posterior fat pad sign may indicate a fracture. [ A lucent crescent of fat in the olecranon fossa on a true lateral view – indicates effusion/hemarthrosis]
A radio-capitellar view may be helpful in doubtful cases (minimally or nondisplaced fractures). This view is taken in neutral rotation & the x-ray tube is angled 45 degrees.
Alternatively, a modified radial-head capitellum view may be taken to identify undisplaced or minimally displaced fractures.
Modified Radial-Head Capitellum view is taken with the posterior aspect of the supinated forearm in contact with the cassette and the elbow slightly flexed. The beam is directed 45 degrees mediolaterally.
CT Scan
Sometimes, CT scanning of the elbow is used to define fracture patterns. CT scan helps in estimating the fracture size, degree of fragmentation, and displacement.
CT should be considered if there are associated elbow injuries, and for planning for surgery in complex injuries.
Treatment of Radial Head Fractures
The goals of treatment of radial head fracture are
- Preservation of elbow motion
- Flexion and extension
- Supination and pronation
- Stability of the elbow joint [in cases where elbow dislocation is present]
Nonoperative Treatment
Fractures with minimum displacement and angulation are treated with nonoperative treatment. This is done by immobilization in a cast or splint followed by physical therapy.
Prolonged immobilization should be avoided as it can lead to elbow stiffness.
Most of the type I fractures respond well to nonoperative treatment.
Type II patients where there is no mechanical block to pronation supination motion can also be treated in this manner.
Operative Treatment
Following surgical treatment options can be exercised depending on patient profile and fracture type
- Fixation after reconstruction of the head
- Partial excision of radial fragments
- Complete excision of radius
- Replacement of radial head by prosthesis
Indications
- Fracture involves more than 33% of the articular surface
- Angulation> 30°
- Displacement > 2-3 mm
- Major loose intra-articular fragments
- Block to pronation and supination
- Presence of associated injuries
- Fractures of the olecranon
- Rupture of the ulnar collateral ligament
- Injury to the distal radioulnar joint
- Interosseous membrane injuring rendering the radius axially unstable
Fixation options include
- K-wires
- Mini fragment plates and screws
- Herbert screws.
When the head cannot be repaired, excision can be considered. If preoperative valgus instability is present medial collateral ligament is repaired.
If there is a concomitant ipsilateral to the distal radioulnar joint injury [Essex Lopresti fracture], the distal radioulnar joint should be repaired.
Replacement surgery should be considered if the fracture is at or below the level of the annular ligament. After surgery, rehabilitation with range-of-motion exercises is begun as soon as the wound is healed. Union usually occurs within 6-8 weeks.
- All type II fractures with a mechanical block are good candidates for fixation.
- Type III radial head fractures are treated with early excision and replacement as comminution jeopardizes the reconstruction of the radial head
- Only excision can be considered in isolated fractures
- Type IV f[those with dislocation], it is preferable to preserve the radial head if possible. Excision should be considered only as a last resort
- If the radial head requires excision, repair of the lateral ligament complex is also required.
- If the radial head cannot be saved and is excised, the potential for redislocation is high.
Complications of Radial Head Fractures
- Infection
- Early or late
- Persistent Pain
- Hardware,
- Cartilage injury
- Posttraumatic arthritis
- Adhesions
- Nonunion and Malunion
- Requires internal fixation or radial head excision or replacement.
- Restriction of Movement
- Synostosis
- Means union to the ulna
- Can occur in closed head injury, delayed surgeries > 2weeks, breach of the interosseous membrane during surgery
- Treated with an interposition spacer
- Proximal Migration of Radius
- Occur in injury to the interosseous membrane
References
- Jackson JD, Steinmann SP. Radial head fractures. Hand Clin. 2007 May. 23 (2):185-93, vi. [Link]
- Rosenblatt Y, Athwal GS, Faber KJ. Current recommendations for the treatment of radial head fractures. Orthop Clin North Am. 2008 Apr. 39 (2):173-85, vi.
- Cooney WP. Radial head fractures and the role of radial head prosthetic replacement: current update. Am J Orthop (Belle Mead NJ). 2008 Aug. 37 (8 Suppl 1):21-5.
- Foocharoen T, Foocharoen C, Laopaiboon M, Tiamklang T. Aspiration of the elbow joint for treating radial head fractures. Cochrane Database Syst Rev. 2014 Nov 22. 11:CD009949.
- Watters TS, Garrigues GE, Ring D, Ruch DS. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis?. Clin Orthop Relat Res. 2014 Jul. 472 (7):2128-35. .