Last Updated on October 20, 2023
Upper cervical spine injury implies injuries to the first and second vertebral regions. The cervical spine is divided into an upper cervical spine which is formed by the atlas (C1), the axis (C2), and adjoining structures. The skull base with its bony and ligamentous elements surrounding the foramen magnum plays an integral part in the maintenance of the normal functional alignment of these two vertebrae.
However, the skull base is not a part of the upper cervical spine.
So the upper cervical spine includes bony and ligamentous structures between the skull base and the cranial side of the C-3 vertebra.
Upper cervical spine injury needs to be addressed separately from the rest of the cervical spine. These injuries are often critical and could be lethal.
Because of complex anatomy and the major role played by ligament stability, this region is quite vulnerable to injury in high-energy trauma. The injuries to these vertebrae and other structures are often associated with neurologic deficits.
Anatomy of Upper Cervical Spine
[Read about the anatomy of the cervical spine]
Read Anatomy of Axis]
The three bony components of the upper cervical spine are the skull base, atlas, and axis. These three components form a functional unit.
Atlas
Atlas or 1 vertebra is the first cervical vertebra that sits just below the skull. It articulates with the dens of the axis, a process of axis vertebra that projects superiorly and the occiput. This articulation is responsible for the rotation of the head.
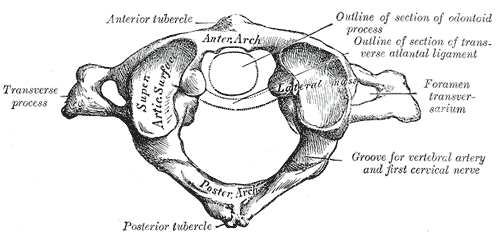
The atlas is composed of
- Anterior arch
- Posterior arch
- Paired lateral masses
- Paired transverse processes
It does not have a body.
[Read Anatomy of Atlas]
Axis or C2
The axis articulates with C1 or atlas vertebra above and the C3 vertebra below.
It forms a pivot for the atlas to rotate providing a greater range of motion than would have been possible otherwise.
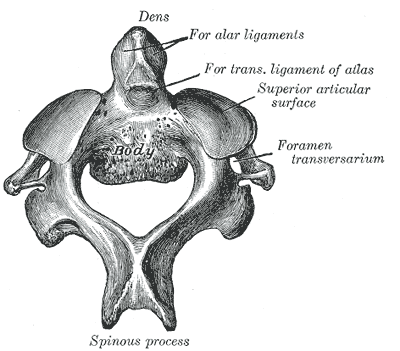
The components of the axis are
- dens
- body
- transverse process
- Superior and inferior articular facets
- pedicle
- lamina
- spinous process.
Joints
- Atlanto-occipital joint – two in number
- Atlanto-axial Joint- Consists of three joints
- atlanto-odontoid joint
- two lateral atlantoaxial joints
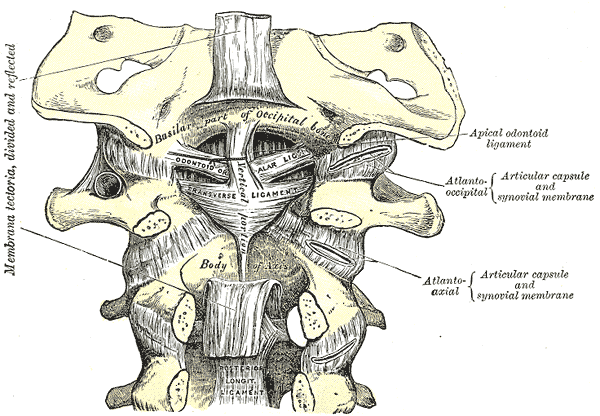
Ligaments and muscles
External ligaments
- Atlanto-occipital
- Anterior longitudinal ligaments.
The internal ligaments are
- The transverse ligament
- connects the medial wall of the anterior third of either lateral mass of the atlas with one another.
- Allows rotation of the atlas on the dens
- stabilizes the cervical spine during flexion, extension, and lateral bending.
- The accessory ligaments
- Are posterior to the transverse ligament
- The apical ligament
- The alar ligaments
- From the medial surface of the occipital condyles to the lateral tip of the odontoid
- Secure the apex of the odontoid to the anterior foramen magnum.
- Prevent excessive lateral and rotational motion while allowing flexion and extension.
- The tectorial membrane
- Continuation of the posterior longitudinal ligament
- Cruciate ligament
- Between the apical ligament and the deep layer of the tectorial membrane
Muscles are divided in 4 groups and play an important role in stability
- Forward flexors are anterior
- Lateral flexors are lateral
- Rotators are lateral
- Extensors are posterior
A high degree of motility and relatively delicate ligamentous and bony structures make the upper cervical spine susceptible to injury from indirect high-energy trauma.
The atlas is the most fragile vertebral segment.
The two most vulnerable bony structures of the axis are the pars interarticularis and the odontoid waist.
Different Types of Upper Cervical Spine Injury
Upper cervical spine injury will consist of injuries to different components of the upper cervical spine. Here, we discuss these injuries one by one briefly
Occipital Condyle Fractures
Occipital condyle fractures are high-energy injuries. Depending on the energy causing them, these can be stable or unstable
If a unilateral bony injury to an occipitocervical joint is identified, the contralateral side should be looked for any signs of a bony or ligamentous injury.
These are commonly associated with ion of occipitocervical dissociation, any occipital condyle fracture should be evaluated for it.
Stable fractures are usually treated conservatively with immobilization in a rigid cervical collar for 6-8 weeks.
Unstable fractures can be managed with a halo vest. However, those with craniovertebral subluxation, some authors advocate immediate occiput-to-C2 fusion.
Occipitocervical Dissociation
Occipitocervical dissociation is a rare injury. A high incidence is seen in children.
Anterior subluxations are most common whereas posterior are rare.
More than 2 mm of translation or distraction in any plane, neurologic injury, or concomitant cerebrovascular trauma should arouse the suspicion of this injury.
Treatment consists of immediate halo vest application with reduction of the subluxation and confirmation by CT scanning.
An occiput-to-C2 fusion is required in most cases to provide long-term stability.
Fracture of C1 Vertebra or Atlas
Atlas fractures can be stable or unstable injuries. This fracture has a very high association with injuries to other areas of the spine.
More than 40% of all C-1 fractures are found to be associated with a C-2 fracture.
Atlas fractures can be of the following types.
- Transverse process fracture
- Posterior arch fracture
- Anterior arch fracture
- Comminuted or lateral mass fracture
- Burst fractures
C2 or Axis Injuries
Fractures of the axis make up about a fourth of all cervical spine injuries.
Different types of injuries to the axis vertebra are
- Odontoid or Dens fractures
- Odontoid fractures account for 10-15% of all cervical fractures.
- Blunt trauma falls
- Can fracture at tip, base or body
- dontoid fractures present with neck pain that worsens with the motion of the neck. Other findings may be motor and sensory neural deficit, dysphagia, and feeling of instability of the head.
- The treatment options are cervical orthosis, halo vest immobilization, surgical fixation, and C1, C2 fusion.
- Hangman Fracture – Traumatic spondylolisthesis of The Axis
- Disruption of the neural arch of the axis.
- May be associated with more complex soft tissue injury
- Motor vehicle accident common cause
- Frequent association with neural deficits
- Treatment
- Stable fractures – 12 weeks of immobilization in a rigid cervical orthosis.
- Mild to moderate instability – skull traction through tongs or a halo ring with a slight extension 3 to 6 weeks, followed by gradual mobilization.
- Highly unstable – open reduction and internal fixation
- Extension teardrop fractures
- Fractures laminae and spinous processes.
Atlantoaxial Injury (Atlantoaxial subluxation)
- Identified as increased mobility between the body atlas and the odontoid process of axis.
- Acute trauma or a direct axial load on the head or cervical spine
- Conditions predisposing
- Odontoid aplasia/ hypoplasia
- Os odontoideum
- Inflammatory disease
- Transverse and alar ligament injury could cause instability.
- Neck pain, stiffness, and torticollis are nonspecific symptoms. Often the condition may not be detected till the time signs of cord compression appear.
- These patients require definitive surgical decompression and instrumented fusion of C1-C2.
[Read more about Atlantoaxial Injury]
Rupture of Transverse Ligament

- A pure ligamentous injury of the upper cervical spine
- Cause- Blows on the back of the head following a fall.
- The ligament avulsion or rupture
- X-rays-
- anterior subluxation of the ring of C1 on lateral views in flexion that mostly reduces on the extension.[Read more about flexion and extension views]
- The presence of retropharyngeal hematoma suggests an acute injury.
- A small fleck of the bone may suggest the avulsion of the ligament.
- Anterior widening of atlantodens interval of more than 5 mm in lateral view in flexion suggests that the transverse ligament is incompetent.
- Initial treatment of this injury is by stabilization of the spine using traction.
- Definitive treatment involves the fusion of C1-C2 vertebrae.
Rotary Subluxation of C1 Vertebra On C2 Vertebra
- This is an uncommon injury in adults, more common in children.
- caused by motor vehicle accidents.
- Presents with torticollis and restricted neck motion.
- An open-mouth view may reveal wink sign due to overriding of the C1-2 joint on one side and normal configuration on the other side.
- Treatment is either by closed reduction or open.
- For closed reduction, after applying a Halo ring, gentle traction is used to derotate the skull and C1 vertebra. Spinal cord monitoring is done throughout the procedure.
- If a stable reduction is obtained, it is confirmed radiologically and a Halo vest is applied.
- Open reduction is done in cases of late detections or failed closed reduction.
Emergency Management of Upper Cervical Injury
The standard protocol of spine injury examination must be followed which includes an assessment of the airway, breathing, and circulation.
The cervical spine should be stabilized immediately in the field and any compromise to the injured spine should be avoided.
High-dose intravenous steroids should be considered in patients with suspected cervical cord injuries to reduce spinal cord swelling.
The patient should be thoroughly examined to find/rule out any other critical injury.
Management of critical injuries takes priority over other things like imaging.
Emergency management is guided by the severity of the injury and the patient’s condition.
Imaging is proceeded with after the patient has been stabilized.
Imaging in Upper Cervical Injury
X-rays
Lateral cervical spine x-ray is the most important trauma screening study. However, the clearance of the cervical spine is not possible on basis of the single lateral plane study. Moreover, the typical lateral cervical spine x-ray is centered in the mid-neck region and the interpretation of the occipitocervical junction can be impaired.
[Read Canadian C-spine Rule]
To be able to rule out injury following bony structures need to be seen on x-ray
- Basion
- Opisthion -On the occipital bone, the mid-point on the posterior margin of the foramen magnum
- Occipital condyles
- Mastoid processes
- Tip of the dens
- Outline of atlas and axis
These structures should be visualized and looked for fracture, rotation, and displacement.
The occipitocervical and atlantoaxial joints should be assessed for congruence.
In adults, the widening of the prevertebral soft tissue mass in the upper neck is an important warning sign of major underlying trauma.
Various Reference lines can help to identify the change in normal upper cervical spine outline.
Anteroposterior visualization of the upper cervical spine requires either an open-mouth odontoid view. Normally, symmetrical articulating occipital condyles, C-1 lateral masses, and C-2 superior articular processes can be visualized. The odontoid is well-centered between the lateral masses of C-1.
Any asymmetry in the context of spinal injury should raise the suspicion of dens fracture, Jefferson fracture, or transverse ligament injury.
Dynamic Radiographs
Dynamic radiographs of the cervical spine are used to find any ligamentous injury to the region.
These may reveal Any odontoid asymmetry relative to the lateral masses of the atlas. A diastasis of the upper cervical spine articulations to one another is cause for suspicion.
Flexion-extension radiographs are contraindicated for patients with known acute cervical spine fractures and dislocations.
In all cases, these x-rays should be done in the presence of physician
Computed Tomography
A head CT scan can be helpful in detecting subarachnoid craniovertebral junction hematoma, which is frequently associated with atlanto-occipital dissociation, and occipital condyle fractures, which are commonly missed on radiography.
- Atlantoaxial rotation of more than 50 degrees in either direction may suggest alar ligament insufficiency.
- > 5 degrees of atlantoaxial flexion indicates transverse ligament insufficiency.
- Atlantoaxial translation > 9 mm in adults craniocervical ligament failure
- If the combined overhang of the C-1 lateral masses relative to the lateral mass walls of C-2 is 7 mm or more, it indicates transverse ligament insufficiency signifies instability.
MRI
Magnetic resonance imaging of the craniovertebral junction is indicated for patients with spinal cord injury, and it can be helpful in assessing upper cervical spine ligament trauma.
Subarachnoid and prevertebral hemorrhage can be readily demonstrated on MRI scans.
MRI provides more detailed imagery of neural and soft tissue.
Nuclear Imaging
Radioisotope-based imaging tests, like technetium-99 bone scan, are rarely required in trauma but can be useful in assessing occult fractures, osteoarthritis affecting the upper cervical spine and in pediatric patients for detection of a nondisplaced growth plate injury.
Treatment of Upper Cervical Spine Injury
The cervical spine is immobilized at the first contact with the patient and is protected throughout the period of evaluation and management of life-threatening conditions if present.
Definite treatment of upper cervical injury depends on the injury and stability of the spine.
For stable injuries, immobilization of the cervical spine is done in a halo vest.
The halo vest consists of a halo and a vest. Halo is a ring that encircles the head and is fixed to it by means of pins that are inserted in the head. It is also known as “halo ring” or “halo crown,”.
The halo ring part of halo vest can be used to put traction on the cervical spine or to provide external support and immobilization.
[Read more om halo-vest immobilization]
Most of the unstable injuries require fusion of C1, C2, and skull, supported by an implant.
Odontoid fractures can also be fixed with screws.
The exact level of fusion would be determined by the level of the injury.
The cervical spine can be approached from the front (anterior) or from the back (posterior).
The posterior approach is more common than the anterior being simpler and extendable cranially and caudally.
The posterior approach is most commonly used in procedures such as
- C-1 laminectomy
- Posterior fossa decompression
- C-2 neurolysis
- C1–2 segment fusion with or without the inclusion of the occiput.
Anterior approaches are used in
- Screw fixation of type II odontoid fracture
- Anterior cervical plating and fusion of the C2–3 interspace for a displaced type IIa hangman’s fracture
- Anterior arthrodesis of the C1–2 facet joints as a salvage
Some of the pathologies of the upper cervical spine are approached through the mouth and the approach is called the transoral approach.
References
- Bransford RJ, Alton TB, Patel AR, Bellabarba C. Upper cervical spine trauma. J Am Acad Orthop Surg. 2014 Nov;22(11):718-29. [Abstract]
-
Liao S, Jung MK, Hörnig L, Grützner PA, Kreinest M. Injuries of the upper cervical spine-how can instability be identified? Int Orthop. 2020 Jul;44(7):1239-1253. [abstract]
-
Pospiech J, Schick U, Stolke D. Indications for surgery in upper cervical spine injury. Neurosurg Rev. 1996;19(2):73-9. [abstract]



