Last Updated on March 15, 2020
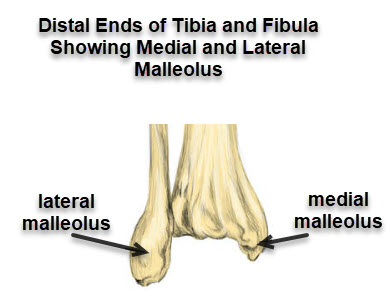
Medial malleolus fracture is a fracture of the distal medial projection of tibia bone called medial malleolus. Medial malleolus and lateral malleolus contribute forms the socket of the ankle joint where talus articulates. There are three malleoli in the ankle. The medial and the posterior arise from the tibia.
A counterpart called lateral malleolus is the distal end of the fibula.
Medial malleolus fracture is a common ankle injury.
Actually, fractures of medial malleolus are part of the spectrum of malleolar fractures and another ankle injuries. It rarely occurs in isolation and is often accompanied by a fracture of lateral malleolus [most common] or posterior malleolus or ligament injury.
Following is an example of undisplaced medial malleolus fracture.

The x-ray shows a fractured medial malleolus.
Like other fractures, treatment depends upon many factors that are injury-related and patient-related. These are the presence of a concomitant fracture of the fibula, amount of displacement of fracture fragments, the age of the patient and demands and expectations of the patient.
The treatment of the medial malleolus fracture can be nonoperative or operative.
Nonoperative treatment or conservative treatment consists of immobilization in below-knee or short leg casts. In some cases, where initial injury has led to substantial swelling, the patient may be given a temporary splint first.
After splinting, the swelling is allowed to reduce before a definitive cast is given.
Nonoperative treatment is mostly done in cases of undisplaced fractures or patients with very low functional demands.
Surgical treatment of medial malleolus fracture aims at anatomical restoration and holding the fractured fragments at that anatomical position by means of screws, K-wires or tension band wiring.
A fractured medial malleolus would take around 4-6 weeks to unite.
Fractures of medial malleolus have a very good prognosis when these are treated appropriately.
A case of Percutaneous Fixation of Medial Malleolus Fracture
The patient had a history of twisting of ankle and broke medial malleolus. Following is the anterior and posterior x-rays of ankle showing the medial malleolus x-ray.

Being an active adult patient and considering the configuration of the fracture, it was decided that the fracture would be fixed. As the fracture was minimally displaced, an attempt to fix the fracture percutaneously without disturbing the soft tissues was made.
The patient was investigated and pre-anesthetic evaluation done.
Spinal anesthesia was used and the patient was kept in a supine position. The limb was externally rotated for better access from the medial side.
The fracture was checked in Carm.
The fracture was held in position with the help of K-wire jockey stick.
The hole for the first screw was drilled after confirming the position in C-arm.
After drilling the hole a malleolar screw was inserted. Here is the preoperative x-ray of the screw being inserted.

Similarly, the second screw was inserted.

After the second screw was inserted, the positions were checked.


The incision sites for screw insertion were stapled.

The immediate postoperative x-ray showed a well-reduced fracture in both AP and lateral views.

The patient was followed up over a period.
Staples were removed after 12 days.
The fracture showed good union on serial x-rays.
Weight-bearing was allowed after 8 weeks of surgery.
Here is an x-ray done after 3 months of surgery.

The fracture is well united and the ankle is well reduced.
Further Study